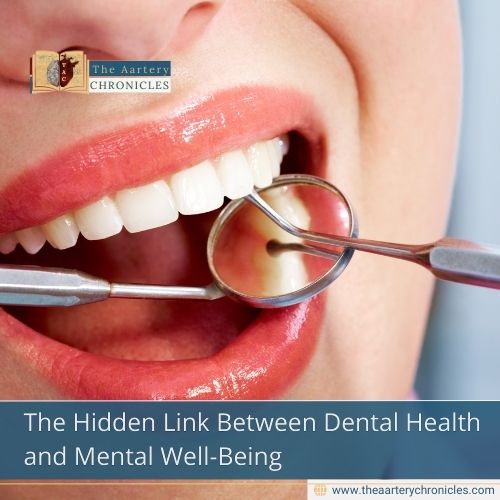
The Hidden Link Between Dental Health and Mental Well-Being
The WHO defined health as “a complete state of physical, mental, and social well-being and not just the absence of disease” (WHO, 1948). As a result, health service researchers have concentrated on health as a multifaceted concept. This notion of health status is based on the biopsychosocial model of health, which integrates physical functioning, emotional and social well-being, and symptoms. People’s “perceptions of their position in life in the context of culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns” (WHOQOL, 1995) are known as quality of life (QoL) , and they are now acknowledged as a valid parameter in patient assessment in almost every area of physical and mental healthcare, including dentistry.
Introduction
Mental health can be impacted by dental disease, or vice versa. An ethical and comprehensive approach to oral health care requires an understanding of the reciprocal or bi-directional relationship between oral and mental health. Increasing awareness, creating ethical and holistic oral health care strategies, and promoting better self-care and help-seeking behaviors all depend on an understanding of this relationship, which will eventually improve treatment outcomes, general well-being, and quality of life (QoL).
According to Antoinette V. Shappell and Pierre M. Cartier, “psychiatrists well understand the need to be aware of all of their patients’ health issues, but sometimes oral health gets overlooked.” Shappell and Cartier highlight the numerous connections between oral and mental health, each of which affects the other. Dental issues can worsen mental health issues and hurt a person’s quality of life.
For example, a person’s eating, speaking, self-esteem, and social relationships can all be negatively impacted by poor oral health, which can further impair mental health. Chronic oral pain can worsen mental health and make treating mental health disorders more challenging, but many people, including those with mental health conditions, have anxiety related to dental care and treatments and avoid necessary care. Mental health symptoms can lead to a poor diet, which can lead to poor oral hygiene.
Oral Health and the Brain: “ The bi-directional connection”
There is a definite link between a person’s mental and oral health, even though this relationship may not be well known. Numerous studies have found links between dental health and mental health, although even medical experts frequently pay little attention to these relationships (1). Moreover, lifestyle changes brought about by mental health problems – such as inadequate diet, excessive carbohydrate consumption, and substance use – could aggravate oral health problems.
How Dental Health and Mental Health Are Connected
Mental illnesses and oral diseases are acknowledged as worldwide public health issues. Anxiety, depression, and schizophrenia are often triggered by systemic inflammation, side effects of medications, and lifestyle changes. These factors significantly affect various aspects of our well-being, encompassing both our oral and physical health. Oral health and mental well-being share a complex and interconnected relationship. Individuals with serious mental illnesses, such as bipolar disorder and schizophrenia, face an increased risk of inadequate dental care and tooth loss stemming from issues like compromised well-being, side effects of psychiatric medications, and ongoing stress. Additionally, lifestyle modifications resulting from mental health issues like poor diet, high carbohydrate intake, and substance abuse may worsen oral health conditions.
The global significance of oral and mental health and their reciprocal link is highlighted by their wide-ranging effects on general health, quality of life, and social well-being, despite the contentious nature of this relationship (2). Both mental and dental health have long been overlooked in the global health agenda, and the connections between mental illnesses and oral diseases, as well as their reciprocal effects on one another. However, people with mental health issues typically have poor oral health and are frequently disregarded because of patients’ lack of drive, ignorance, low socioeconomic position, phobias, and dentists’ unwelcoming attitudes.
Dental Anxiety and Depression: The Hidden Cycle
Anxiety and depression symptoms are commonly associated with psychological distress, which is a significant public health issue. Dental anxiety causes avoidance behaviours and poor oral health, which is a major obstacle to receiving dental care. Psychologically distressed patients may have poor oral hygiene habits that result in poor oral hygiene and dental diseases.
Higher age, low income, health issues, and smoking were all associated with psychological discomfort. Oral hygiene, gingival health, and dental caries experience were all substantially connected with psychological distress (3).
The greatest effect of anxiety or dental phobia is seen in the inconsistency or avoidance of regular dental appointments, which in turn exacerbates oral health issues. Bad oral hygiene adversely impacts social well-being and self-worth. Individuals with chronic oral health issues experience psychological distress. This parallelism highlights the importance of fostering the connection between mental health and oral health to improve the quality of life for these individuals. These factors are associated with socioeconomic issues, restricted access to dental services, and diminished overall health in people with mental health disorders. Financial issues, stigma concerns, and the absence of integrated care models are some reasons many individuals with mental health conditions refrain from seeking dental services.
Studies indicate that dental problems, including periodontitis, can lead to systemic inflammation, exacerbating mental health conditions such as anxiety and depression. Likewise, unaddressed mental health issues may lead to neglect of dental care, creating a cycle of worsening health (4).
The role of the microbiome
The complete group of microorganisms that live in a specific habitat, including bacteria, viruses, fungi, archaea, and even protozoa, is referred to as the microbiome. The term “microbiome” refers to both the creatures and their collective genetic material, whereas “microbiota” refers to the organisms themselves.
Over 700 microbial species make up the oral microbiome, which supports gum and dental health but, when out of balance, can lead to periodontal disease and tooth decay. Changes in the gut microbiota have been linked to mental health conditions such as autism spectrum disorders, anxiety, and depression. The research indicates that microbiological health may have an impact on psychological well-being; these relationships are still being worked out.
The gut microbiota has been shown to play a significant role in regulating mental health and brain function. It has been demonstrated that the gut microbiota can encourage the emergence of mental illnesses, including anxiety and depression (5).
The relationship between gut microbiome and depression has been found and reported. The two-way communication between the gut and brain has been proposed as a potential foundation for their interrelation. The central nervous system (CNS) is influenced by the gut microbiome through metabolites produced by microbes and neurotransmitters like γ-aminobutyric acid (GABA) and serotonin (5-hydroxytryptamine, 5-HT). Growing evidence indicates a significant role of the microbiota–gut–brain axis in depression (6). Oral microbiome, being the second-largest microbiota in humans, is closely associated with the progression of different pathological conditions. It was noted that, since the gut was connected to the oral cavity, the microbes in the oral cavity contributed significantly to the development of the gut microbiota
Fitness and Nutrition Angle
Nutrition plays a crucial role in improving and managing athletic performance, and post-exercise dietary advice is essential for recovery and adaptation processes. Athletic nutrition can significantly affect oral health because of higher intake of energy gels, bars, and sports beverages. Higher consumption and regular eating occasions involving dental exposure to carbohydrates, free sugars, sports nutrition items, and acidic, carbohydrate-laden sports beverages elevate the likelihood of dental erosion, cavities, and inflammatory periodontal diseases, particularly in situations of dehydration and inadequate oral care. Untreated cavities and severe caries can lead to widespread infection, impacting the health and performance of athletes. Specifically, top athletes with a compromised immune system and elevated cortisol levels from stress, demands, and overload, alongside added dental and/or periodontal inflammation, face the risk of dental diseases (8).
The provision of food and fluids is essential for achieving peak athletic performance, yet it can also contribute to the risk of dental caries, erosion, and periodontal diseases, which may negatively affect athletic performance. Numerous studies have indicated a significant occurrence of oral diseases among athletes, particularly with dental caries ranging from 20-84%, dental erosion from 42-59%, gingivitis from 58-77%, and periodontal disease from 15-41%, attributed to the frequent intake of sugars/carbohydrates, polyunsaturated fats, or insufficient protein consumption. The three primary factors contributing to the poor oral health observed in athletes are oxidative stress, sports nutrition, and oral hygiene practices (9).
Conclusion
Models of integrated care that combine dental and mental health services have demonstrated effectiveness in enhancing oral health results, particularly for at-risk populations. Both oral and mental health issues should be fully addressed by the interdisciplinary cooperation of dentists and other medical specialists to create awareness and improve the overall well-being of the patients.
Effective mental health care contributes to maintaining good oral health by encouraging regular dental hygiene habits. Likewise, public health initiatives might leverage this information effectively for prevention, lowering healthcare expenses, and enhancing patient outcomes.
Source: Inputs from various media Sources
- Asiri, A., Nazir, M.A., Alsharief, M. et al. Effect of psychological distress on oral health: a cross-sectional study. BMC Oral Health 24, 1508 (2024).
- A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson NW. Psychosom Med. 2015;77:83–92.
- Association between mental health and oral health status and care utilization. Tiwari T, Kelly A, Randall CL, Tranby E, Franstve-Hawley J. Front Oral Health. 2021;2:732882.
- Oral health of adults with serious mental illnesses: a review. Matevosyan NR. Community Ment Health J. 2010;46:553–562.
- Peirce JM, Alviña K. The role of inflammation and the gut microbiome in depression and anxiety. J Neurosci Res. 2019 Oct;97(10):1223-1241. doi: 10.1002/jnr.24476. Epub 2019 May 29. PMID: 31144383.
- Lou F, Luo S, Kang N, Yan L, Long H, Yang L, Wang H, Liu Y, Pu J, Xie P, Ji P, Jin X. Oral microbiota dysbiosis alters chronic restraint stress-induced depression-like behaviors by modulating host metabolism. Pharmacol Res. 2024 Jun;204:107214. doi: 10.1016/j.phrs.2024.107214. Epub 2024 May 17. PMID: 38763328.
- S.Y. Park, B.O. Hwang, M. Lim, S.H. Ok, S.K. Lee, K.S. Chun, et al.Oral-Gut Microbiome Axis in Gastrointestinal Disease and Cancer Cancers, 13 (9) (2021).
- 8.Needleman I., Ashley P., Petrie A., Fortune F., Turner W., Jones J., Niggli J., Engebretsen L., Budgett R., Donos N., et al. Oral health and impact on performance of athletes participating in the London 2012 Olympic Games: A cross-sectional study. Br. J. Sports Med. 2013;47:1054–1058.
- Schulze A, Busse M. Sports Diet and Oral Health in Athletes: A Comprehensive Review. Medicina (Kaunas). 2024 Feb 13;60(2):319. doi: 10.3390/medicina60020319. PMID: 38399605; PMCID: PMC10890155.
- Z K, Siluvai S, Kanakavelan K, Agnes L, Kp I, G K. Mental and Oral Health: A Dual Frontier in Healthcare Integration and Prevention. Cureus. 2024 Dec 23;16(12):e76264.
ASLIN SANOFER
- TAC Desk
- Health News and Updates,People Forum
- 6 January 2026
- 11:00