Sleep is the Honest Mirror of a Fractured Mind: Insomnia as a Public Symptom
Summary
This article explores insomnia as a reflection of societal stress and systemic imbalance, arguing that sleeplessness is less a personal flaw and more a public symptom demanding collective attention. Drawing on historical, philosophical, and medical perspectives, it highlights how economic insecurity, social isolation, and discrimination drive rising rates of insomnia especially among the most vulnerable. The piece calls for compassion and systemic reform, reframing insomnia from an individual burden to a societal challenge rooted in shared responsibility.
The Vanishing Memory of Restful Sleep And A Global Epidemic of Insomnia
When was the last time you really slept well and woke up feeling fully refreshed? That answer is a distant memory for millions. Too frequently, our society views restless nights as the result of bad behavior or a lack of self-control. But what if insomnia is a truthful mirror of how society itself has lost its direction, rather than just a personal error?
Globally, insomnia is now an epidemic. Studies by the World Health Organization and sleep organizations indicate a significant increase in sleeplessness, which is often linked to financial instability, widening social divides, and the relentless nature of digital connection. These restless evenings are a group cry for assistance, not only individual difficulties.
In many respects, sleep acts like a sensitive seismograph for society. While entire communities lie awake night after night, gazing at the ceiling, their racing thoughts indicate not only the effects of caffeine or blue-lit screens but also concerns about paying rent, mourning broken communities, and the stressful unpredictability that permeates modern life. Insomnia is a warning, not only a symptom.
A Historical Perspective on Sleeplessness
Philosophers and storytellers have always understood the more profound significance of insomnia throughout history. Ancient Stoics regarded insomnia as proof of internal disturbance. Expanded work hours and urban populations brought about by the Industrial Revolution made sleeplessness a lived reality for the working classes. Insomnia in our time corresponds strongly with employment insecurity, social isolation, and even the destabilizing effects of climate change. Every night without sleep bears echoes of financial changes, moving street lights, and missing social safety nets.
The Limits of Popular Advice
Popular advice rarely conveys the whole picture in spite of this complexity. “Sleep hygiene” recommendations, meditation apps, and melatonin gummies rule the market as though insomnia were just a technical issue to be solved by better routines. Still, this tactic can be subtly malicious, assigning guilt to people while ignoring the disruptive environments around them. Increasingly, sleep medicine specialists and scientists emphasize how strong drivers of pervasive insomnia are chronic stress, economic hardship, racism, and discrimination. Statistically, those residing in impoverished areas, battling continual uncertainty, or suffering prejudice are much more likely to have persistent sleep loss.
Maya’s Story: A Mirror of Modern Struggles
Let’s talk about Maya, a devoted schoolteacher trying to juggle two jobs in the face of growing living expenses. Late into the evening, her head races with anxieties about expenses, the futures of her students, and the safety of her surroundings. For Maya, insomnia shows the daily balancing act demanded by contemporary systemic imbalances rather than a lack of willpower. Her narrative represents millions: sleep loss is often a sensible reaction to an absurd world.
The Ripple Effects of Insomnia
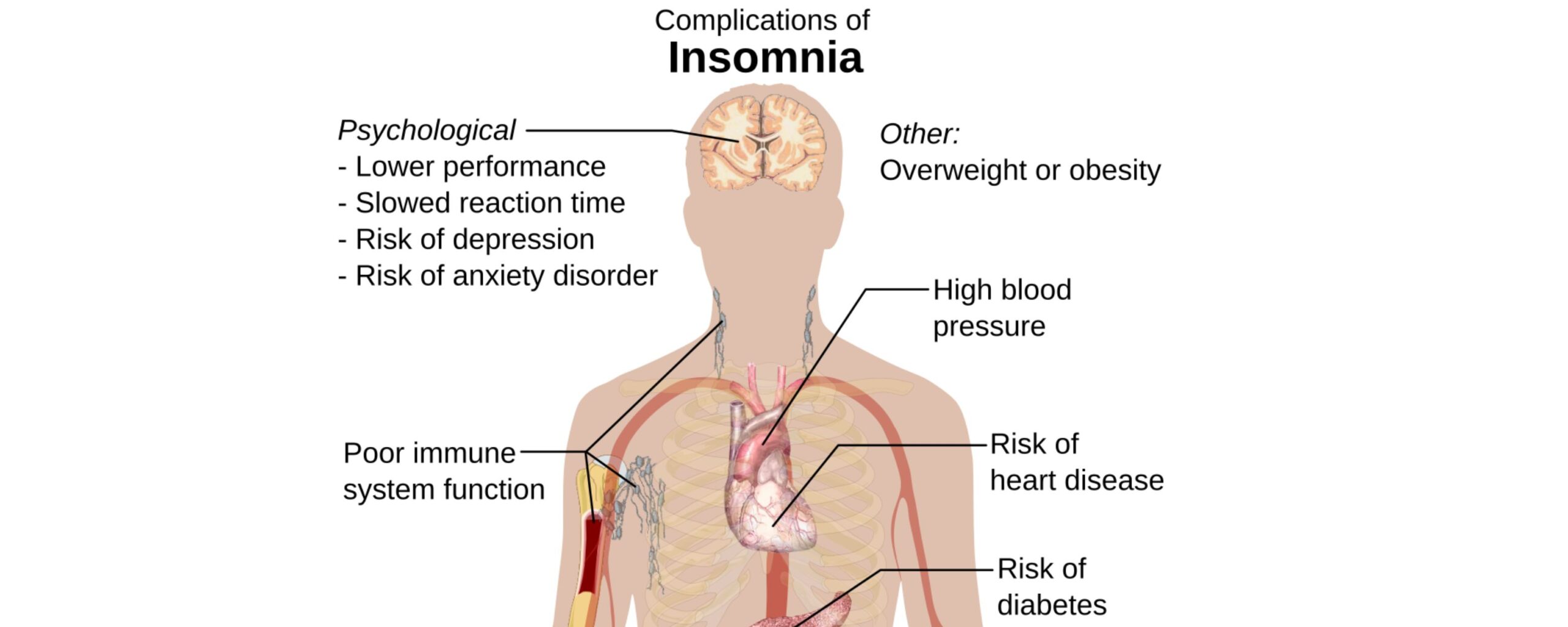
Insomnia spreads its influence to all aspects of life. Chronic insomnia worsens despair, worsens anxiety and depression, damages focus and memory, and harms mental health. Downstream effects are workplace mistakes, traffic accidents, and frayed relationships. Though it appears to be entirely personal, what might seem like a very private fight is actually extremely public, costing governments billions in healthcare expenses and lost production.
Still, the lived reality of insomnia is frequently moralized. These phrases, “If you just tried harder,” “Avoid screens,” “Stick to a routine”, are familiar to anybody who has ever confessed their nighttime difficulties. But such treatments create guilt, isolation, and self-blame while concealing the truth, sleeplessness is a gauge of the fault lines passing through society itself.
What Is Insomnia Trying to Tell Us?
Thus, what is insomnia trying to tell us? Should whole populations be unable to sleep, what reality about our current situation are we missing? Our common inability to rest raises challenging issues regarding the stresses of labor that do not stop after sunset, the solitude created by urban design and overstretched schedules, and the silent despair of individuals unable to afford housing, safety, or time for recuperation.
Instead of condemnation, we need compassion, not just for the insomniacs among us but for the root causes that keep us all from rest. Rather than individual remedies, we need group ones, reasonably priced healthcare, community-based mental health care, workplace reform, and regulations addressing housing, education, and systemic inequality. Should sleepless nights be a choir of anxiety, their answer rests not only in the doctor’s office but also in social activity, political will, and the restoration of broken communities.
Sleep as a Mirror of Society
Sleep is ultimately the clear reflection of a damaged mind and a broken world. Society speaks when it cannot sleep off what has been lost, missed, or broken. Considering sleep deprivation as a reflection of society assists in healing both ourselves and the systems we reside in.
The question remains, “Will we listen?”
- https://www.aamc.org/news/sleep-determinant-health
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8494094/
- https://jcsm.aasm.org/doi/10.5664/jcsm.10336
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4987093/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10788304/
- http://sleepmedres.org/journal/view.php?doi=10.17241%2Fsmr.2024.02152
- https://jcsm.aasm.org/doi/10.5664/jcsm.9476
- https://pmc.ncbi.nlm.nih.gov/articles/PMC647387
- https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(23)00182-2/fulltext
- Dr Yashvi Singh
- Public Health
- 17 September 2025
- 11:00
Reviewed by Dr Aarti Nehra (MBBS, MMST), & Dr Darshit Patel (MBBS)