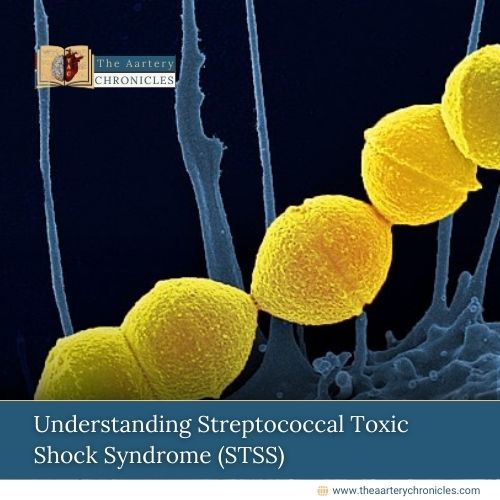
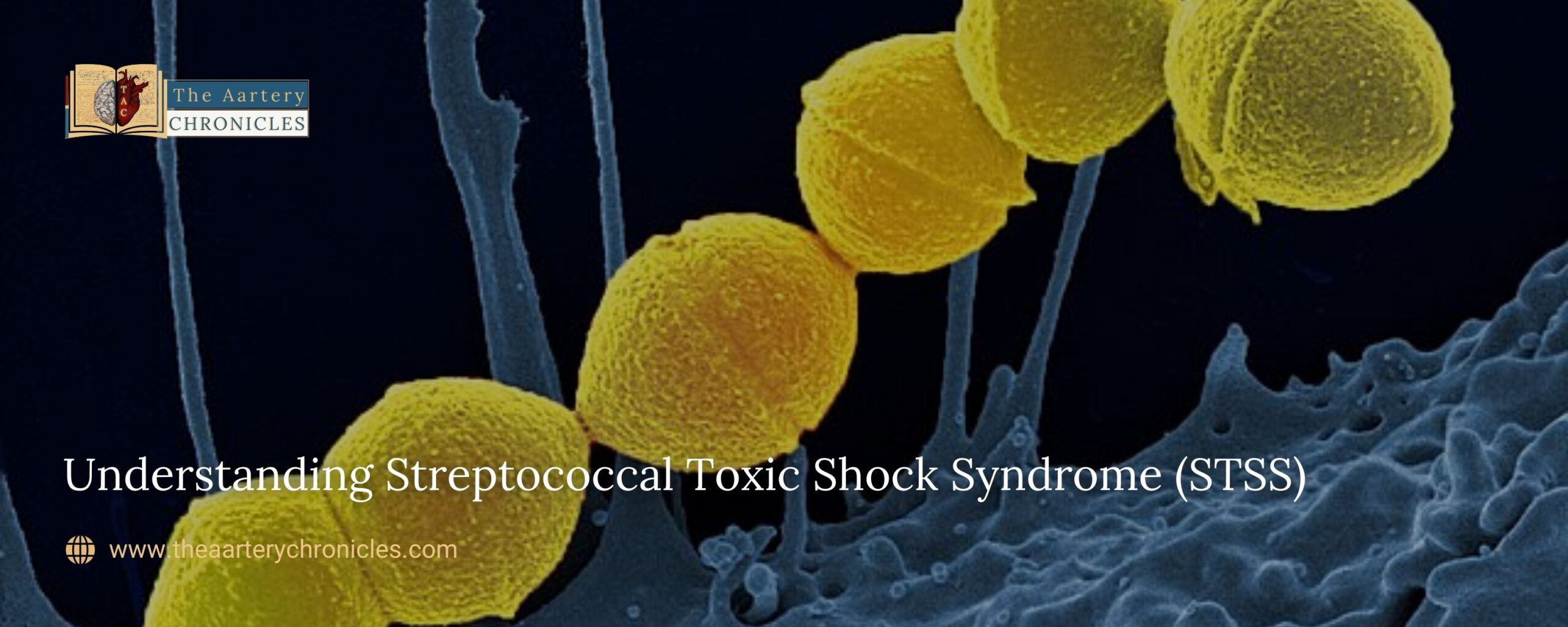
Understanding Streptococcal Toxic Shock Syndrome (STSS)
Surge in STSS Cases in Japan
Recently, Japan has been experiencing an unprecedented surge in cases of Streptococcal Toxic Shock Syndrome (STSS). As of early June this year, the number of cases has already surpassed the 1000 mark, compared to around 941 cases recorded annually in 2023.
Experts suggest that the sudden increase in cases may be due to the lifting of restrictions post-COVID pandemic and reduced immunity among the population. The relaxation of these restrictions led to a decline in the continuous use of masks, hand sanitizing, and adherence to the “three Cs” (closed spaces, crowded places, and close-contact settings) which had significantly helped in controlling COVID-19 cases in the country.
What is Streptococcal Toxic Shock Syndrome (STSS)?
Streptococcal Toxic Shock Syndrome (STSS) is a severe acute condition caused by infection with an invasive strain of Group A Streptococcus (Streptococcus pyogenes). The disease is characterized by the sudden onset of shock and organ failure, and it has a fatality rate that can exceed 50%. [1]
Streptococcal Toxic Shock Syndrome (STSS) is a type of Toxic Shock Syndrome (TSS) both of which are caused because of toxin-producing bacteria, particularly Streptococcus pyogenes, Staphylococcus aureus, and, Clostridium sordellii. [2]
Toxic Shock Syndrome (TSS) is a potentially fatal condition caused by bacterial strains, including Streptococcus pyogenes and Staphylococcus aureus, which produce toxins that can damage organs such as the kidneys, liver, and heart. TSS is often associated with tampon use during menstruation, making it more common in females, and it can affect up to 1 in every 100,000 people. [3]
Cause and Incubation Period
Toxic Shock Syndrome (TSS) occurs when certain bacteria, such as Streptococcus pyogenes and Staphylococcus aureus, produce virulence factors and exotoxins that enter the bloodstream and deep tissues, triggering a cytokine cascade.
- This cascade can lead to multiple organ failure and the development of shock. The bacterial strains responsible for producing these exotoxins and virulence factors are associated with severe infections.
The incubation period for TSS can vary depending on the site of bacterial entry.
- After the onset of symptoms, hypotension typically develops within 24 to 48 hours.[4]
Signs and Symptoms
STSS can commence with influenza-related signs such as
- Fever
- Chills
- Nausea
- Myalgia
The disease can eventually advance and result in sepsis with
- Shock
- Bleeding problems
- Flat and red rashes covering most body areas
- Skin shedding in large sheets particularly soles and palms
- Breathing difficulties
- Bruising because of low platelet count
- Hypotension
- Tachypnoea
- Tachycardia
- Specific symptoms associated with failure of organs.
- Organ systems including blood, lungs, liver, and kidneys may fail [2] [4]
The loss of extremities (amputation) and tissue necrosis may be the common complications known for organ failure and shock. [4]

Risk factors for Streptococcal Toxic Shock Syndrome (STSS)
- Age: Anyone can contract STSS, but it is most frequently observed in adults over 65 years old.
- Open Wounds: Individuals with open wounds, such as those from surgery, or infections that cause open sores, including shingles and chickenpox, are at an increased risk.
- Health Conditions: Certain health factors, such as diabetes and alcohol dependence, can also increase the risk of developing an STSS infection. [4]
Diagnosis of of Streptococcal Toxic Shock Syndrome (STSS)
The diagnosis of STSS is primarily determined through the isolation and identification of specific strains of bacteria from blood cultures. The diagnosis is based on the Council of State and Territorial Epidemiologists (CSTE) 2010 case definition, which requires the following criteria:
- Multi-Organ Involvement: Evidence of involvement of multiple organ systems.
- Isolation of Bacteria: Isolation of Group A Streptococcus (Streptococcus pyogenes) from a normally sterile site, such as blood, cerebrospinal fluid, or pleural fluid.
- Hypotension: The presence of hypotension (low blood pressure).
By meeting these criteria, a diagnosis of STSS can be confirmed. [4, 5]
Treatment of Streptococcal Toxic Shock Syndrome (STSS)
As a first step, fluid resuscitation is crucial for treating organ failure and shock. Specific treatment options are determined by the healthcare provider based on the following factors:
- Extent of Disease: The severity and spread of the infection.
- Patient’s Tolerance: The patient’s tolerance to specific procedures, therapies, and medications.
- Other Factors: Considerations such as age, medical history, and overall health.
These individualized treatment plans help optimize the management and recovery of patients with STSS. [4]
The treatment options for STSS may involve the following:
- Antibiotics and Therapies: Intravenous administration of antibiotics, such as clindamycin and penicillin, is considered the primary first-line treatment. Other required therapies may also be administered intravenously.
- Medications and Treatments for Specific Organs: Depending on the organ systems affected, treatments may include heart medications for cardiac issues and dialysis for kidney failure.
- Intravenous Immunoglobulin (IVIG): For patients with severe symptoms, IVIG may be considered during the early clinical course, although its efficacy has not been conclusively proven. [2,4]
- Surgical Procedures: Surgical removal of infected sources is often necessary in managing STSS. This may include surgical debridement to treat deep tissue infections. [4]
These combined approaches aim to manage the infection, support organ function, and improve patient outcomes.
Preventive Measures for Streptococcal Toxic Shock Syndrome (STSS)
Preventive measures to reduce the risk of STSS include:
- Awareness and Public Health Education: Increasing awareness about STSS and educating the public on prevention and early symptoms.
- Good Hygiene Practices: Regular hand washing, proper wound care, and maintaining cleanliness.
- Using Preventive Antibiotics: In some cases, prophylactic antibiotics may be recommended to prevent infections.
- Limiting Exposure and Spread of Infection: Avoiding contact with infected individuals and taking precautions to prevent the spread of bacteria.
- Washing Clothes, Towels, and Linens: Washing these items daily and avoiding sharing them to prevent the spread of infection.
- Immediate Treatment for Streptococcal Infections: Seeking prompt medical treatment for streptococcal infections to prevent complications.
- Care for Fungal Infections: Properly treating fungal infections to prevent secondary bacterial infections.
- Careful Observation of Skin Infections and Wounds: Monitoring skin infections and wounds for any signs of infection and seeking prompt treatment if needed.
These preventive measures help reduce the risk of developing STSS and other related infections. [4] [6]
- Streptococcal Toxic Shock Syndrome (STSS) (Streptococcus pyogenes) 1995 Case Definition | CDC
- Toxic Shock Syndrome (TSS) | Johns Hopkins Medicine
- Toxic Shock Syndrome | Cleveland Clinic
- Clinical Guidance for Streptococcal Toxic Shock Syndrome | CDC
- Streptococcal Toxic Shock Syndrome: A Case Report | NCBI
- Preventing Group A Strep Infection | CDC
Sanika Pande
- Medicine and Diseases
- Nutrition and Diet