Lung Abscess: Pathophysiology, Diagnosis, and Management
Excerpt
A lung abscess is a purulent inflammation of the lung parenchyma leading to cavitation. It is a serious condition that can arise from infectious and non-infectious causes. This article explores its pathophysiology, clinical manifestations, diagnostic methods, treatment approaches, and surgical interventions. A clinical case is also presented to illustrate the real-world challenges of managing lung abscesses.
ICD Codes and HCC Classification
- ICD-10 Code: J85.2 (Lung abscess with pneumonia)
- HCC Code: HCC 112 (Chronic Lung Disease)
- Related Codes:
- J85.1 (Abscess of lung without pneumonia)
- R22.1 (Localised swelling, mass, or lump of the thorax)
Definition
Lung abscesses develop due to bacterial invasion, leading to tissue necrosis and pus formation. The condition progresses in two stages:
- Acute stage: Before rupture into the bronchial system, the abscess is walled off and contains purulent material.
- Chronic stage: Following rupture, inadequate drainage can lead to persistent infection and fibrosis.
Complications include thromboembolism (due to deep vein thrombophlebitis), pulmonary infarction, and empyema if the abscess ruptures into the pleural cavity.
Aetiology and Risk Factors
Common Causative Organisms
- Anaerobic bacteria: Peptostreptococcus, Fusobacterium, Bacteroides
- Aerobic bacteria: Staphylococcus aureus, Klebsiella pneumoniae, Pseudomonas aeruginosa
- Fungal and Mycobacterial Causes: Aspergillus, Nocardia, Mycobacterium tuberculosis
Risk Factors
- Aspiration risk: Alcoholism, seizures, stroke, dysphagia
- Immunocompromised states: Diabetes, HIV, malignancy
- Pulmonary conditions: Chronic obstructive pulmonary disease (COPD), bronchiectasis
Symptoms and Signs
Acute Lung Abscess
- High fever (>38°C)
- Dry cough
- Shortness of breath (SOB)
- Pleuritic chest pain
- Generalised intoxication symptoms
Chronic Lung Abscess
- Persistent cough with large amounts of purulent sputum
- Low-grade fever (subfebrile)
Diagnosis
Laboratory Tests
- Urinalysis: Similar to other suppurative infections
- Blood tests: Leukocytosis with neutrophilia, elevated inflammatory markers (CRP, ESR)
- Biochemical tests: Assess metabolic and immune responses
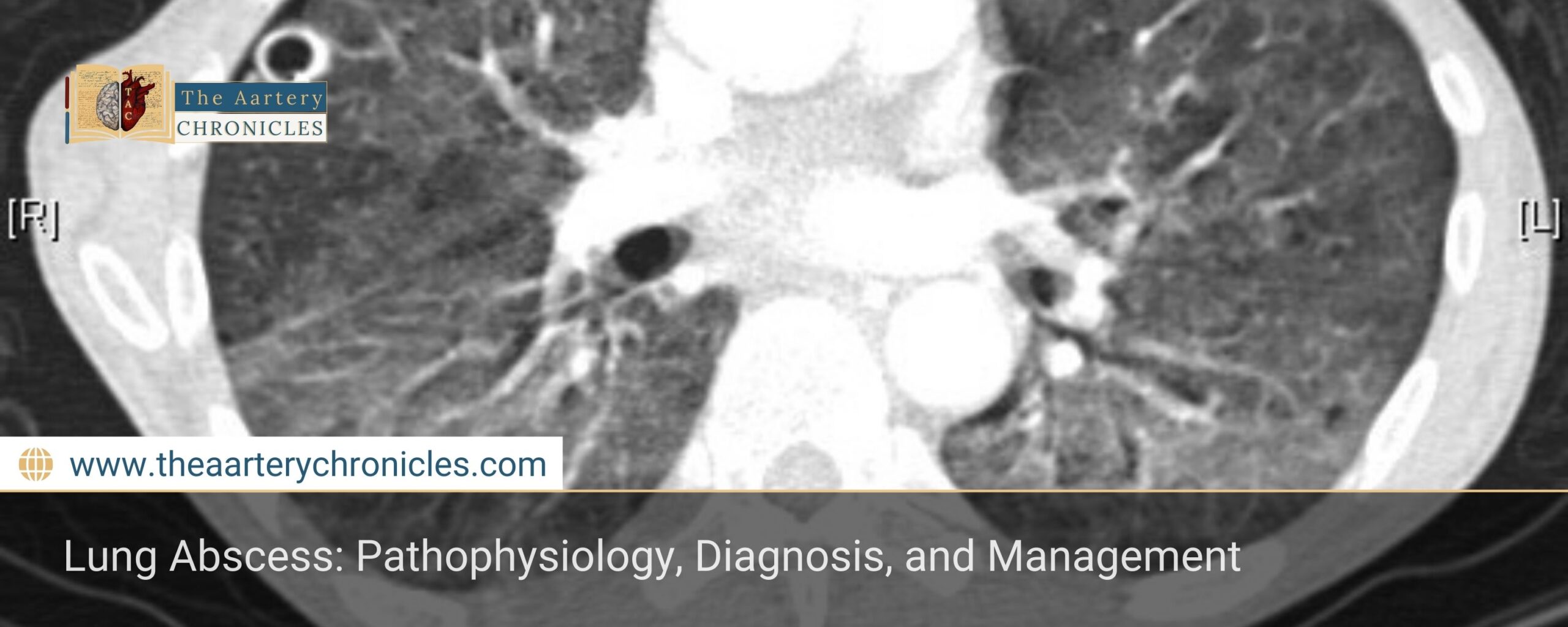
Imaging
- Chest X-ray: Reveals a fluid-filled cavity with a surrounding capsule
- CT Scan: More sensitive for detecting abscess localisation and assessing adjacent structures
Differential Diagnosis
Lung abscess must be distinguished from:
- Lung Tumour: No fluid or gas in the lesion; lacks fever and malaise; may present as nodular growth
- Tuberculosis (TB): Typically affects the upper lobe of the right lung, presents with hemoptysis rather than purulent sputum, and has a diffuse “snow-like” lung appearance
Treatment
Conservative Management
- Before opening into the bronchial system: IV antibiotics and detoxification therapy
- After opening into the bronchial system, Antibiotics with effective drainage of pus
Pharmacological Treatment
- Empirical Antibiotic Therapy (covering anaerobes and Gram-negative bacteria):
- Piperacillin-tazobactam 4.5 g IV every 6 hours OR
- Meropenem 1 g IV every 8 hours (for resistant cases) OR
- Clindamycin 600 mg IV every 8 hours (if anaerobic infection is suspected) + Ceftriaxone 2 g IV once daily
- Oral Step-Down Therapy (after clinical improvement):
- Amoxicillin-clavulanate 875 mg/125 mg PO twice daily OR
- Levofloxacin 750 mg PO once daily (if beta-lactam allergy present)
- Supportive Care:
- IV fluids and electrolyte balance
- Antipyretics (Paracetamol 1 g PO/IV every 6 hours as needed for fever)
- Oxygen therapy if hypoxia
Surgical Interventions
Surgical intervention is considered when conservative treatment fails:
- Bronchoscopy: Direct aspiration and lavage of the cavity with antibiotics
- Percutaneous Drainage: Insertion of a trocar under radiological guidance to evacuate pus and instil antibiotics
Statistical Data
- Incidence: Approximately 0.5–0.9 per 100,000 individuals per year
- Mortality rate: 5–10% in treated cases; up to 30% if complications arise
- Common pathogens: Anaerobic bacteria (e.g., Fusobacterium, Bacteroides), Staphylococcus aureus, and Klebsiella pneumoniae.
Clinical Case
Patient Profile:
- A 47-year-old male, a chronic smoker, presented with high-grade fever, severe cough, and right-sided pleuritic pain.
Findings:
- Chest X-ray: Large cavitary lesion with air-fluid level in the right lung
- CT Scan: Confirmed an abscess in the right lower lobe with adjacent pleural thickening
Treatment & Outcome:
- IV Piperacillin-tazobactam 4.5 g every 6 hours
- Bronchoscopic aspiration of pus
- Oral step-down to Amoxicillin-clavulanate 875 mg/125 mg PO twice daily for 4 weeks
- Gradual improvement over 3 weeks with resolution of fever and improved radiographic findings
Mnemonic for Causes of Lung Abscess:
"A BAD ASPIRATION"
- Anaerobes (Fusobacterium, Bacteroides)
- Bacterial pneumonia (Staphylococcus aureus, Klebsiella pneumoniae)
- Aspiration (alcoholics, unconscious patients, seizures)
- Diabetes mellitus
- Abnormal lung structure (bronchiectasis, COPD)
- Sepsis (hematogenous spread)
- Post-obstructive pneumonia (tumour, foreign body)
- Immunosuppression (HIV, steroid use)
- Rheumatoid arthritis (necrotising pneumonia)
- Atypical infections (TB, fungi)
- Thromboembolism (septic emboli)
- Intubation/ventilation (aspiration risk)
- Obstructive lung diseases (chronic bronchitis, bronchial stenosis)
- Neoplasms (leading to secondary infection)
Mnemonic for Clinical Features of Acute Lung Abscess
"F-PODS"
- Fever (>38°C)
- Pleuritic chest pain
- Ongoing dry cough
- Dyspnea (shortness of breath)
- Systemic intoxication (malaise, weakness)
Mnemonic for Clinical Features of Acute Lung Abscess
"PUS"
- Persistent cough with purulent sputum
- Unresolved low-grade fever
- Subacute presentation
References

Author
Dr Darshit Jagdish Patel








