
Arthritis Awareness: Understanding Symptoms, Types, and Management Strategies
Introduction
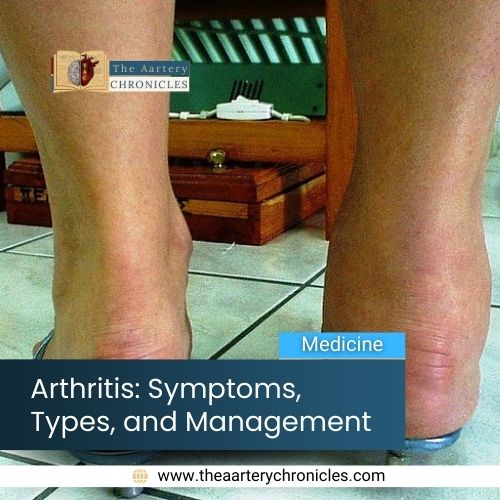
Arthritis is an umbrella term that encompasses more than 100 different arthritic conditions that affect joints and are a chronic, painful, and debilitating group of diseases. In 2019, roughly 528 million individuals worldwide were affected by osteoarthritis, representing a surge of 113% from the numbers recorded in 1990. [1, 2]
May is observed as Arthritis Awareness Month, a time dedicated to raising awareness about arthritis and related conditions. Arthritis Awareness Month serves as an opportunity to highlight the prevalence of arthritis across all age groups, dispel myths and misconceptions surrounding the condition, and advocate for improved access to healthcare services, research funding, and effective treatments. It also emphasizes the importance of adopting healthy lifestyle habits, such as maintaining a balanced diet, staying physically active, managing stress, and seeking regular medical check-ups to prevent or manage arthritis effectively. [3]
In this article, we aim to explore the multifaceted nature of arthritis, delving into its intricate details such as symptoms, types, risk factors, and essential management strategies. Understanding these aspects is pivotal for early detection and intervention, ensuring effective management of the condition.
What is Arthritis?
The term “arthritis” directly translates to “inflammation of the joints.” Arthritis is a chronic medical condition characterized by inflammation of joints leading to pain, stiffness, swelling, and decreased mobility. It encompasses a wide range of conditions, including osteoarthritis, rheumatoid arthritis, gout, lupus-related arthritis, and psoriatic arthritis. [2, 4, 5]
Body Parts Affected by Arthritis
Arthritis primarily affects the joints, but depending on its type, it can also impact other structures such as surrounding tissues, muscles, ligaments, tendons, and even internal organs in some autoimmune forms. Joints affected by arthritis primarily include:
- Hands
- Wrists
- Hips
- Knees
- Feet and ankles
- Shoulders
- Spine (lower back) [6]

Types of Arthritis
As individuals age, some joints naturally undergo wear and tear over time, leading to the development of arthritis in many cases. Additionally, certain types of arthritis can arise from injuries that result in joint damage, while specific health conditions can also contribute to the onset of arthritis.
Different types of arthritis affect specific joints and tissues in varied ways, influenced by factors such as ageing, injury-related wear and tear, inflammation, genetic predisposition, or the body’s immune system response. Of the numerous variants of the condition, some of the most common types of arthritis include:
- Osteoarthritis (OA): Osteoarthritis is the most common form of arthritis, often referred to as “wear and tear” or “degenerative” arthritis. OA commonly affects weight-bearing joints such as the knees, hips, and hands.
- Rheumatoid Arthritis (RA): Rheumatoid arthritis is an autoimmune disorder where the immune system mistakenly attacks healthy cells of the body. RA typically affects smaller joints first, such as those in the hands and feet, but it can progress to larger joints over time.
- Gout: Gout is a form of inflammatory arthritis caused by the deposition of uric acid crystals in the joints. This condition typically manifests as sudden and severe pain, swelling, redness, and tenderness in the affected joint. It commonly affects one joint at a time, commonly the big toe.
- Ankylosing Spondylitis: Ankylosing spondylitis, also referred to as axial spondyloarthritis, is an inflammatory condition that gradually leads to the fusion of certain spinal bones, known as vertebrae. This fusion reduces spine flexibility and can lead to a stooped or hunched posture.
- Psoriatic Arthritis (PsA): Psoriatic arthritis (PsA) is a chronic inflammatory condition that affects both the skin and joints and results in pain, stiffness, and swelling in the affected joints. PsA often coexists with psoriasis, a persistent autoimmune skin disorder characterized by an accelerated skin cell growth cycle. [2, 4,6, 7]
What are the Signs and Symptoms of Arthritis?
The symptoms of arthritis can vary depending on the type and severity of the condition. However, common symptoms include:
- Joint Pain
- Stiffness
- Swelling
- Reduced joint mobility
- Skin discoloration
- Tender to touch around the joint
- Sensation of heat or warmth near the affected joint [6]
Some other symptoms of osteoarthritis include:
- Pain or discomfort in a joint during or after activity, especially following prolonged activity or at the end of the day.
- Stiffness in the joint is typically experienced upon waking in the morning or after periods of rest.
- Reduced ability to move the joint fully, which may improve with movement
- Audible clicking or popping sensation when the joint bends.
- Visible swelling around the joint
- Weakness in the muscles surrounding the joint
- Joint instability or buckling [8]

What are the Risk Factors for Arthritis?
While arthritis can impact anyone, there are certain factors that increase the likelihood of developing the condition, such as the use of tobacco, smoking, genetic predisposition, lack of physical activity, and the presence of concurrent health issues like autoimmune diseases and obesity.
Some people who are at an increased risk of developing arthritis include:
- Individuals aged 50 and above
- Individuals assigned female at birth (AFAB)
- Athletes, particularly those engaged in contact sports
- Individuals with physically demanding occupations or tasks that place significant strain on their joints (such as prolonged standing, crouching, or being on hands and knees for extended periods) [6]
How is Arthritis Diagnosed?
Arthritis is diagnosed through a combination of medical history, physical examination, imaging tests, and laboratory tests. The healthcare provider will likely assess range of motion, which measures how far one can move a joint. They may compare the range of motion in one joint to that of other similar joints.
Imaging tests used to detect arthritis encompass X-rays, ultrasound, magnetic resonance imaging (MRI), and computer tomography (CT) scans. These examinations enable healthcare providers to visualize internal joint damage. If gout is suspected, a healthcare provider may conduct blood tests to measure uric acid levels. Additionally, blood tests can reveal indications of infections or autoimmune conditions. [6, 9]
Management Strategies for Arthritis
While there is no cure for arthritis, healthcare providers will assist in finding treatments to manage symptoms. The specific treatments required depend on the underlying cause and type of arthritis, as well as the affected joints.
- Medications
- Over-the-counter (OTC) nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation.
- Disease-modifying antirheumatic drugs (DMARDs) are often prescribed for rheumatoid arthritis to slow disease progression and preserve joint function.
- Corticosteroids, including cortisone shots, are commonly used as a treatment for arthritis.
- Physical Therapy
- Physical and occupational therapy can play an important role in the management of some types of arthritis. Physical therapy exercises can help improve joint flexibility, strength, and range of motion.
- Surgery
- Joint Repair: In this procedure joint surfaces can be realigned or smoothed to alleviate pain and enhance function. These procedures are frequently conducted arthroscopically, using small incisions near the joint.
- Joint Replacement: This surgical intervention involves the removal of the impaired joint and its substitution with an artificial counterpart. The hips and knees are the most commonly replaced joints.
- Joint Fusion: This procedure is typically employed for smaller joints like those found in the wrist, ankle, and fingers. It entails removing the ends of the two bones within the joint and then locking the ends together until they fuse into a single rigid unit. [6, 9]
Conclusion
In conclusion, arthritis is a widespread condition that affects millions worldwide, characterized by joint inflammation, pain, and reduced mobility. Its multifaceted nature demands a comprehensive approach to management, blending medical interventions, lifestyle adjustments, and emotional support. Despite the hurdles it presents, ongoing research and advancements in treatment offer hope for improved outcomes and quality of life for those affected. By fostering awareness, support, and collaborative efforts, we can strive towards a future where arthritis is better understood, effectively managed, and its burdens lightened for all.
- Osteoarthritis (who.int)
- Arthritis Types | CDC
- Arthritis Awareness Month | Arthritis Foundation
- Arthritis Basics: Overview, Symptoms, and Causes (nih.gov)
- Arthritis - Symptoms and causes - Mayo Clinic
- Arthritis: Symptoms, Causes, Types, Treatment & Prevention (clevelandclinic.org)
- Ankylosing spondylitis - Symptoms & causes - Mayo Clinic
- Osteoarthritis: Symptoms, Diagnosis, and Treatment | Arthritis Foundation
- Arthritis - Diagnosis and treatment - Mayo Clinic
- Prevalence of arthritis according to age, sex and socioeconomic status in six low and middle income countries: analysis of data from the World Health Organization study on global AGEing and adult health (SAGE) Wave 1 - PMC (nih.gov)