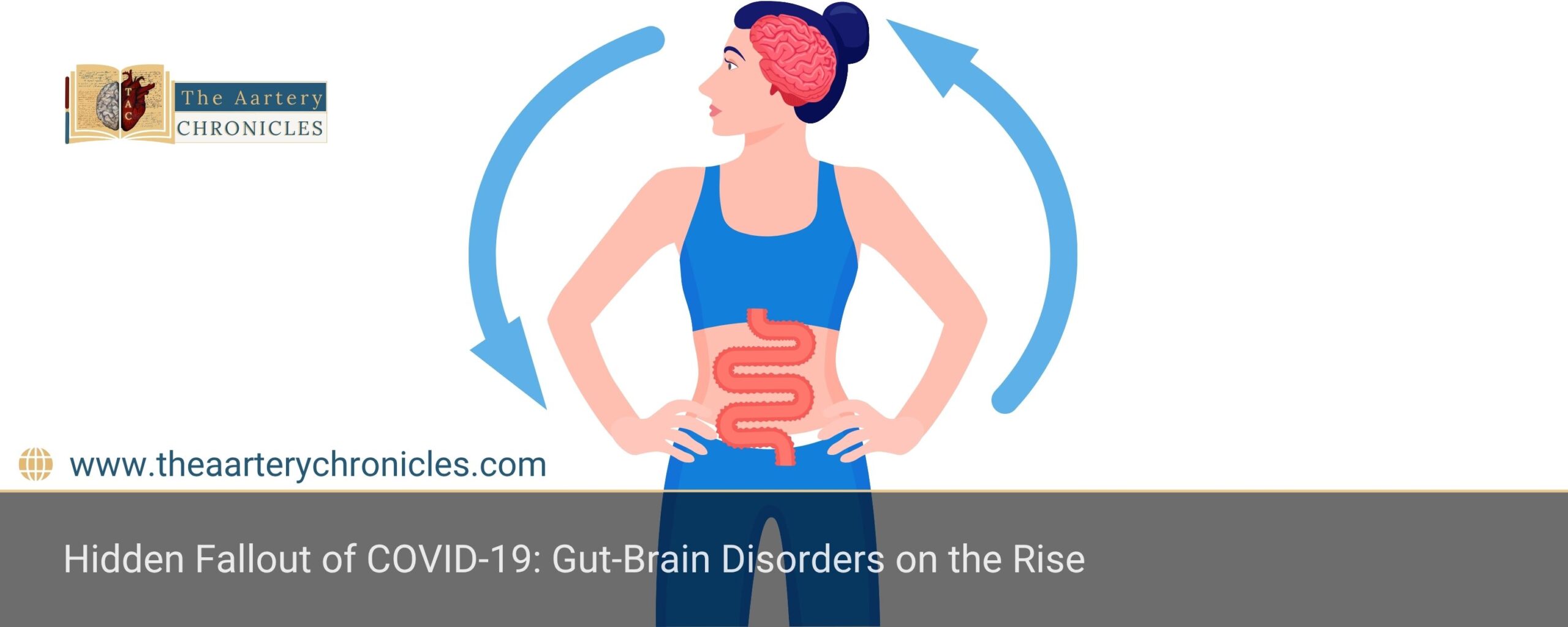
Hidden Fallout of COVID-19: Gut-Brain Disorders on the Rise
Summary: New research from around the world is showing a pretty noticeable jump in gut-brain issues like IBS and indigestion after COVID, especially in folks dealing with long COVID. This emphasises how much we need to focus on mental health and digestive care right now.
Gut-Brain Disorders Surge Post-COVID, Especially in Long COVID
Did you know that issues like irritable bowel syndrome (IBS) and functional dyspepsia have really taken off since the COVID-19 pandemic hit?
A recent international study found that these gut-brain problems became a lot more common between 2017 and 2023. The increase is especially noticeable in individuals dealing with long COVID, who also tend to report higher levels of anxiety, depression, and a lower quality of life.
Study Confirms Sharp Post-COVID Spike in DGBIs
This study, published in Clinical Gastroenterology and Hepatology, is the first large-scale study to look at how gut-brain disorders have changed before and after the pandemic, using the consistent diagnostic tools from the Rome Foundation.
It provides us with some interesting numbers to consider:
- Overall, gut-brain issues increased from 38.3% to 42.6%.
- Specifically, IBS cases increased by about 28%, jumping from 4.7% to 6%.
- Functional dyspepsia saw a 44% rise, increasing from 8.3% to 11.9%.
- Plus, people dealing with Long COVID tend to be at higher risk of these problems and often face more severe mental health challenges.
IBS: A Disruptive Yet Underdiagnosed GI Disorder
Irritable Bowel Syndrome (IBS) is a long-term condition that messes with your stomach and guts. Some of the main symptoms people experience are
- Abdominal pain
- Feeling bloated
- Diarrhoea, constipation, or both
Even though it’s not deadly, IBS can really throw a wrench into your daily routine. Experts think it’s all about a tricky connection between your gut and brain, which affects how your digestion works and how sensitive you are to discomfort, plus, stress can make it worse. Usually, doctors diagnose it based on how you feel (using the Rome IV criteria), and managing it often involves
- Changing what you eat (like trying low FODMAP diets or adjusting fibre intake)
- Finding ways to handle stress better
- Sometimes, taking specific medications to help control symptoms
Functional Dyspepsia: When the Gut Feels Full Too Soon
Functional dyspepsia is a common issue that affects the upper part of your digestive system. Some typical symptoms you might notice include
- Feeling pain or discomfort in your upper belly
- Feeling full fast even after just a little bit of food
- Experiencing nausea
- Feeling bloated
Unlike conditions like ulcers or GERD, there’s no obvious structural problem causing these symptoms. It’s actually thought of as a gut-brain interaction issue, which means it could be linked to
- Motility issues
- Visceral hypersensitivity
- Psychological stress
When it comes to managing it, most individuals find that making changes to their diet and daily habits helps, along with psychological therapies like CBT or relaxation techniques.
Sometimes, doctors might recommend medications such as proton pump inhibitors (PPIs), medicines that help your stomach move better (prokinetics), or even antidepressants to help with symptoms.
Long COVID Might Make the Gut-Brain Link Even More Sensitive
People dealing with long COVID have been noticing more issues with how their gut and brain communicate, along with common mood struggles like anxiety and depression. This suggests that COVID-19 could be messing with the gut-brain connection, affecting
- Immunity
- The bacteria in our guts
- How our nervous system functions
Why This Study Really Matters
This is actually the first big study looking at both pre- and post-pandemic data on gut-brain issues, using the same consistent methods. It gives stronger evidence that long COVID could be behind some of the ongoing health problems many people are facing after recovering from the virus.
The Way Forward: Rethinking GI and Mental Health Care
The data calls for:
- Updated care models that integrate gastroenterology and psychiatry
- Greater research into gut-brain mechanisms post-infection
- Targeted screening for long COVID patients
By acknowledging the pandemic’s hidden effects on the gut-brain axis, clinicians can better support patients struggling with post-COVID symptoms
Wrapping-up
COVID-19 didn’t just mess with our lungs, it affected other parts of our health, too. We’ve seen more cases of gut-brain issues like IBS and functional dyspepsia, especially in individuals dealing with long COVID. This really emphasises how we need to look at health in a more all-around way, focusing on integrated care that covers everything, not just isolated symptoms.
Dane
I am an MBBS graduate and a dedicated medical writer with a strong passion for deep research and psychology. I enjoy breaking down complex medical topics into engaging, easy-to-understand content, aiming to educate and inspire readers by exploring the fascinating connection between health, science, and the human mind.








