Trauma and DID: Key Insights into Dissociative Identity Disorder
The Role of Trauma in the Development of Dissociative Identity Disorder (DID)
Trauma as a Primary Factor
Trauma is widely recognized as a significant contributing factor to Dissociative Identity Disorder (DID).
- The disorder often emerges as a coping mechanism in response to overwhelming stress or trauma, particularly during formative years.
- According to research, a high percentage of individuals with DID have experienced severe and chronic childhood abuse, including physical, emotional, or sexual abuse.
- The trauma induces a state of dissociation, where the individual mentally distances themselves from the traumatic experience. This dissociation can become so ingrained that it results in the formation of multiple distinct alters, each representing different aspects of the person’s identity and experiences.
Mechanisms of Dissociation
Dissociation serves as a defense mechanism, allowing individuals to compartmentalize traumatic memories and emotions. When faced with unbearable situations, the person may feel as if they are observing the trauma from a distance or that it is happening to someone else. This process of detachment helps to reduce the immediate psychological impact of the trauma. Over time, if the trauma is ongoing or repeated, dissociation can lead to the fragmentation of the self, resulting in the development of different alters that hold and manage different aspects of the trauma.
Neurological Changes
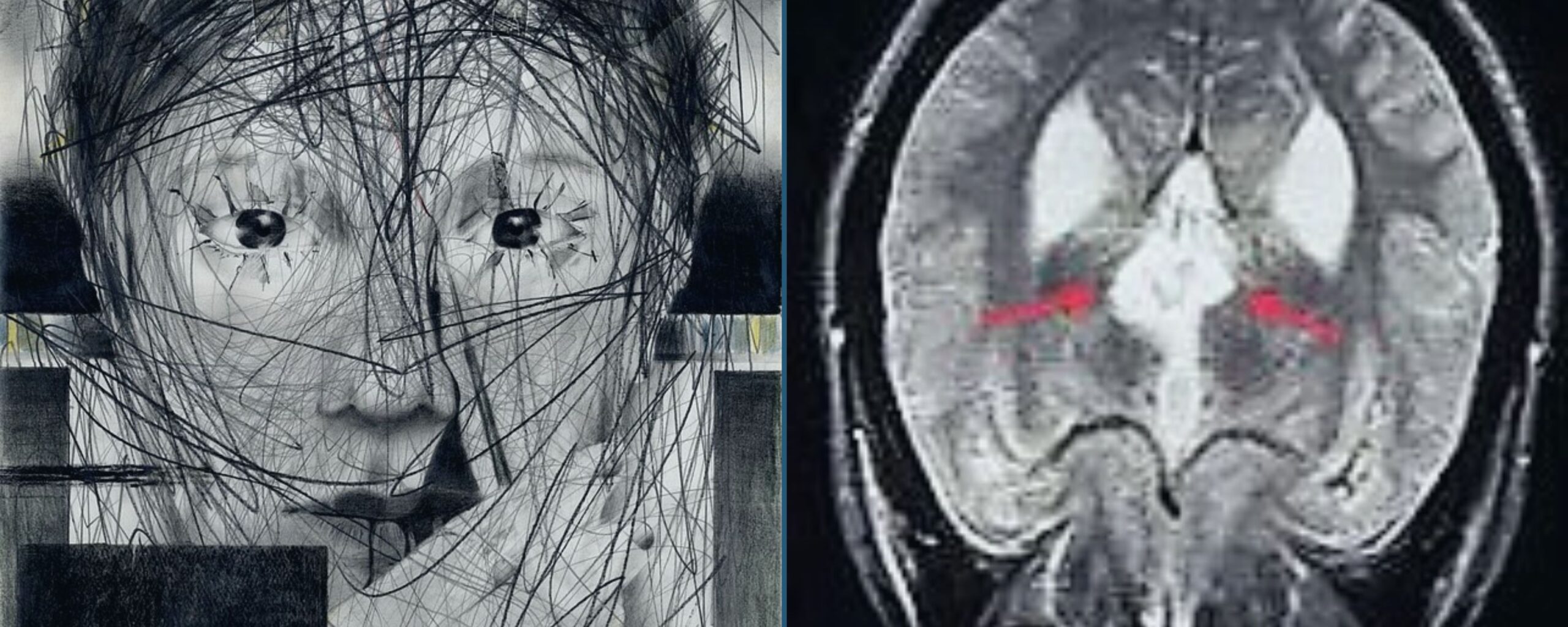
Research has indicated that trauma can lead to neurological changes in the brain.
- Studies have shown that individuals with DID may have differences in brain structures related to memory and self-perception. For instance, findings have linked trauma to alterations in the hippocampus and other brain regions associated with memory processing and emotional regulation.
- These changes can influence the formation and maintenance of alters, as well as the individual’s overall cognitive and emotional functioning.
Variability in Trauma Responses
Not all individuals who experience trauma develop DID. The development of the disorder is influenced by various factors, including
- The nature of trauma
- Frequency
- The severity of the trauma
- Individual’s genetic predisposition
- Family environment
- Coping mechanisms
This variability highlights the complexity of DID and suggests that while trauma is a significant factor, it interacts with other personal and contextual elements to contribute to the development of the disorder.
The application of Schema Therapy (ST) for treating Dissociative Identity Disorder (DID)
Schema therapy is an integrative psychotherapy approach that addresses deep-seated patterns and beliefs formed early in life to treat complex psychological conditions.
A study reported the benefits of schema therapy in treating Dissociative Identity Disorder (DID) through the following methods:
- Case Study: Involving a 43-year-old woman with symptoms of DID.
- Treatment Methodology: Comprised of 220 schema therapy sessions tailored for DID.
- Approach:
- Developed a personalized model.
- Managed dissociative responses using grounding techniques and physical cues.
- Addressed avoidance behaviours with creative solutions.
- Reframed substance use as avoidance.
- Trauma Processing: Utilized Imagery Rescripting (ImRs) to progressively handle traumatic memories.
- Results: Significant improvements in PTSD and dissociative symptoms, enhanced social functioning, and reduced suicidal behaviours.
- Conclusion: Indicates schema therapy may be a valuable alternative for treating DID.
Symptoms of Dissociative Identity Disorder (DID)
DID is characterized by the presence of two or more distinct personality states or identities, each with its own pattern of perceiving and interacting with the world. Key symptoms include
- Severe dissociative amnesia, where individuals experience significant memory loss not due to medical conditions
- Dissociative fugue, which involves sudden, unplanned travel and amnesia of personal information
- Blurred identity, is where the person feels like multiple distinct identities or personalities are interacting within their mind. Each identity may have unique attributes, such as different names, ages, or even physical characteristics.
Treatment for Dissociative Identity Disorder (DID)
The primary treatment for DID is psychotherapy, which involves talking with a mental health professional to understand and manage the disorder. This can include techniques like
- Cognitive-behavioural therapy
- Trauma-focused therapy
Hypnosis may also be used as an adjunct treatment. Although there are no medications specifically approved for DID, medications such as anti-anxiety drugs, antipsychotics, or antidepressants might be prescribed to address associated symptoms. The focus of treatment is often on integrating the separate identities and processing traumatic memories.
Recent advancements in the understanding and treatment of Dissociative Identity Disorder (DID):
- Neuroimaging Studies: Recent neuroimaging studies have identified structural and functional brain differences in individuals with DID, providing evidence that supports the existence of distinct identities. These findings help substantiate the disorder’s clinical presentation and highlight the neurobiological underpinnings of dissociation.
- Trauma Research: Advances in trauma research have reinforced the link between severe and chronic childhood trauma, particularly abuse, and the development of DID. This connection underscores the importance of addressing trauma in therapeutic approaches and offers insights into the disorder’s origins.
- Diagnostic and Therapeutic Advances: Efforts to improve diagnostic accuracy include the development of standardized assessment tools, such as the Structured Clinical Interview for Dissociative Disorders (SCIDD). These tools aim to enhance the precision of DID diagnoses and reduce the risk of misdiagnosis. Therapeutically, integration therapy remains a primary approach, focusing on consolidating the separate identities into a cohesive whole. Despite ongoing debates about its effectiveness, it continues to be a major method of treatment.
Case Study: Dissociative Identity Disorder (DID) in an 18-Year-Old Woman
A case study detailed by Dr. Eric K. Mason focuses on an 18-year-old woman with Dissociative Identity Disorder (DID). She witnessed her mother’s death and was raised by her grandmother following this traumatic event. The case reported no known history of mental illness or significant medical issues prior to this incident.
Behavioral Observations
- Physical Appearance: The young woman appeared undernourished and fainted during a clinical interview when exposed to cold water. Despite her frail appearance, she demonstrated notable physical strength.
- Behavioral Issues: She exhibited frequent incidents of stealing and lying, such as taking money and a pocket knife. When questioned, she claimed that the stolen items were either found or given to her by someone else.
- Inconsistent Behavior: The woman displayed behaviors typical of a younger child, including stealing money to buy candy and seeking affection in a manner reminiscent of a much younger individual.
- Memory Gaps and Inconsistencies: Her accounts of events contained contradictions, particularly regarding interactions with a neighborhood boy and another girl. These inconsistencies suggest possible shifts in identity.
Diagnostic Criteria
- Presence of Distinct Identities: The woman’s behaviors and statements indicate multiple identities or personality states.
- Recurrent Control by Different Identities: Her shifts in behavior and memory gaps suggest that different identities may control her actions at different times.
- Inability to Recall Important Information: Her denial of thefts and inconsistencies in her stories indicate significant memory gaps.
- Exclusion of Other Conditions: The symptoms cannot be attributed to substance use, general medical conditions, or mere fantasy play.
Diagnostic Justification
- Behavioral Shifts: Observations of her erratic behavior and requests for affection typical of a younger child align with the presence of alternate identities.
- Memory Gaps: Denials of witnessed events and contradictory statements support the notion of dissociative memory gaps.
- Family Dynamics: Her background, including potential neglect and emotional abuse from her grandmother, aligns with common DID etiological factors.
Conclusion
The disorder’s link to severe trauma underscores the importance of addressing both the psychological and neurobiological aspects of treatment. Despite ongoing debates about the effectiveness of various therapeutic approaches, such as Schema Therapy and integration therapy, the focus remains on improving diagnostic accuracy and treatment efficacy.
The case study of the 18-year-old woman exemplifies the complexities of DID and highlights the necessity for continued research and specialized training for mental health professionals. With advancements in neuroimaging, trauma research, and diagnostic tools, there is hope for more effective management of DID. By continuing to dispel myths and advancing our understanding, we can enhance the quality of life for individuals affected by this challenging disorder.

Abhigyan Barooah
Reviewed by Dr. Aarti Nehra