Cotard’s Syndrome: All that You Need to Know
Opioid Overdose Complicated by Cotard’s Syndrome
A 41-year-old male patient was brought to the emergency department in a comatose state after an opioid overdose at a Halloween party. His Glasgow Coma Scale score was <8, respiratory rate <10, and PaO2 <60 mm Hg. The patient’s vitals were stabilized, and Naloxone was administered. After 36 hours, he was transferred to the general ward, where he refused treatment, believing that his organs did not exist and that he would soon die. Physicians, unable to understand his condition, called the on-call psychiatrist.
After speaking with the patient and his family, the psychiatrist diagnosed him with Cotard’s syndrome, a rare psychiatric disorder often associated with severe depression. Unfortunately, the patient passed away a few weeks later due to starvation
What is Cotard’s Syndrome?
Cotard’s Syndrome is a rare psychiatric disorder characterised by delusional beliefs, where patients may feel that they are dead, immortal, or lacking internal organs, despite evidence to the contrary. These patients often experience self-destructive thoughts, leading to an increased risk of suicide.
Delusions in Cotard’s Syndrome
- In some cases, the mind may create delusions of being the cause of all the wrong in the world. For example, one patient believed there was poison inside him, and urinating might harm everyone in the hospital.
- Conversely, some patients may blame the world for the wrongs they perceive have happened to them.
Diagnostic criteria and Associated Disorders in Cotard’s Syndrome
Cotard’s Syndrome does not have a specific definition or diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM). It is considered a delusional symptom that can occur as part of other conditions such as
- Bipolar disorder
- Chronic depression
- Schizophrenia
- Cerebral atrophy
- Temporal lobe disorders
- Epilepsy
It is also observed in patients with substance abuse.
Hallucinations and Self-Monologues
Additionally, some patients may experience self-monologues or auditory hallucinations, and both auditory and visual hallucinations can be present.
Stages of Cotard’s Syndrome
Cotard’s Syndrome is typically described in three stages:
- Stage 1 – The Germination Stage
This stage is marked by hypochondriacal delusions and cenesthopathy. Hypochondriacal delusions involve the belief that the patient has a serious underlying illness. Cenesthopathy refers to strange bodily sensations, such as feeling as though there is a foreign object (e.g., a wire or coil) in the body, such as the oral cavity. - Stage 2 – The Blooming Stage
In this stage, patients experience nihilistic delusions, such as believing they are dead, immortal, or that their internal organs are absent or decaying. - Stage 3 – The Chronic Stage
The chronic stage can be divided into two types: depressive and paranoid. The depressive type involves emotional disturbances, with depressive symptoms often becoming less prominent over time. The paranoid type may involve delusions of persecution or extreme mistrust.
Diagnosis of Cotard’s Syndrome
The diagnosis of Cotard’s Syndrome is primarily made through a detailed conversation with the patient about their experiences and beliefs. The key complaints reported by patients include:
- They do not exist.
- Internal organs are absent from their body.
- They are immortal.
- The inside of their body is rotten.
These patients often have other neurological disorders, which may contribute to the development of Cotard’s Syndrome due to brain damage.
Nihilistic Beliefs and Associated Data
Nihilistic beliefs, such as denial of one’s existence, body parts, environment, or other people, are central to Cotard’s Syndrome. A study on patients with Cotard’s Syndrome revealed the following associations:
- 86% had delusions related to their own body.
- 65% felt guilt.
- 58% experienced hypochondriacal delusions.
- 55% had delusions of mortality.
- 89% and 63% experienced depression and anxiety, respectively.
Prevalence of Cotard’s Syndrome
Cotard’s Syndrome is extremely rare. In a 2013 Australian study by Stompe and Schand, only 3 out of 346 schizophrenic patients were diagnosed with Cotard’s Syndrome.
Neurobiological Findings
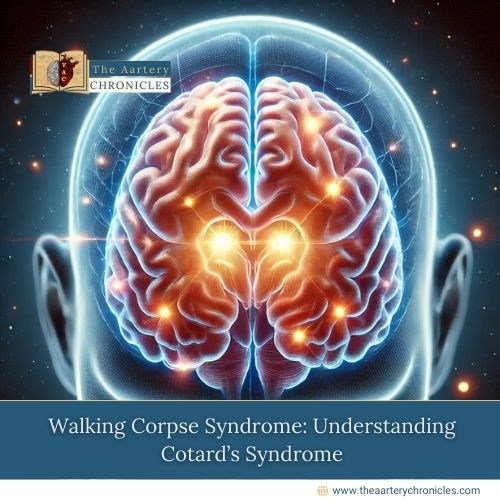
Neurobiological research has shown that there is a loss of connection between the fusiform area and the amygdala in the brains of patients with Cotard’s Syndrome. The fusiform area is responsible for recognizing facial features, while the amygdala is the center for emotional processing. This disconnection leads to the recognition of one’s face without experiencing any emotional connection or self-worth.
Additionally, a decrease in hippocampal volume has been observed in patients with Cotard’s Syndrome.
Treatment of Cotard’s Syndrome
The initial treatment of choice for Cotard’s Syndrome is pharmacotherapy, which may involve antipsychotics alone or in combination with antidepressants or mood stabilizers. The primary goal is to address both the psychotic and depressive symptoms.
Electroconvulsive Therapy (ECT)
Electroconvulsive therapy (ECT) is considered when pharmacotherapy fails. A Japanese meta-analysis study showed that ECT had a 21.6% effectiveness rate in treating Cotard’s Syndrome in 130 cases.
Preferred Medications
The preferred drugs for treating Cotard’s Syndrome include Olanzapine and Fluoxetine.
- Olanzapine: This atypical antipsychotic has a high affinity for Dopamine D2 and Serotonin 5-HT2A receptors. It helps alleviate psychotic symptoms by regulating dopamine and serotonin levels in the brain.
- Fluoxetine: A selective serotonin reuptake inhibitor (SSRI), Fluoxetine is responsible for neuroplasticity and neuroprotection. Neuroplasticity aids in healing from psychotic and depressive episodes by reorganizing neural circuits, which helps in improving mood and cognition.
The Takeaway
With awareness of its stages and treatment options, it is possible to manage and treat patients with Cotard’s Syndrome, as demonstrated in the Japanese studies. While Cotard’s Syndrome is rare, its impact on patients can be profound. Early recognition and intervention are crucial for improving outcomes. Therefore, more research and the development of effective treatment strategies are essential to address its unique challenges, reduce its devastating effects, and enhance the quality of life for affected individuals.
2. Fusick AJ, Davis C, Gunther S, Klippel C, Sullivan G. Psychotropic Management in Cotard Syndrome: Case Reports Supporting Dual Medication Management. Case Rep Psychiatry. 2024 Apr 9;2024:7630713. Available at: https://pubmed.ncbi.nlm.nih.gov/38633733/