Everything you need to know about Parkinson's Disease
Parkinson’s disease is a gradual degenerative neurological condition characterized by movement impairments, typically affecting individuals over the age of 60. According to worldwide data from 2019, more than 8.5 million people were diagnosed with Parkinson’s disease. In India, the estimated number of individuals living with Parkinson’s was approximately 0.58 million in 2016, with a projected significant rise in prevalence anticipated in the near future.
What is Parkinson’s disease?
Parkinson’s disease (PD) is a chronic neurological condition characterized by the loss or impairment of dopamine-producing neurons in the midbrain. This neuronal damage is often attributed to the accumulation of abnormal proteins, leading to the classic triad of symptoms:
- Tremors (shaking)
- Rigidity (stiffness)
- Bradykinesia (slowness of voluntary movements)
Types of Parkinson’s disease
There are several types of Parkinson’s disease based on their origin:
- Primary/Idiopathic: This type is the most common type that accounts for 80-85% of cases and the exact cause of cell death is unknown.
- Secondary or acquired: This type is caused by underlying factors such as drugs, toxins, infections, tumors, or trauma. It is relatively uncommon.
- Familial: This type is caused by inherited genetic mutations and accounts for approximately 15% of cases.
- Early-Onset Parkinson’s: This rare form of Parkinson’s affects individuals between the ages of 21 and 40, comprising about 10% of cases.
What is the Cause of Parkinson’s disease?
Parkinson’s disease is marked by a reduction in dopamine production caused by the loss of cells in the substantia nigra due to accumulation of abnormal protein. This leads to compromised communication with neurons in the basal ganglia, which play a primary role in coordinating movements.
Basal Ganglia
The basal ganglia is a complex network of structures located deep within the brain. It plays a vital role in coordinating voluntary movements and regulating motor functions. By transmitting nerve signals to muscles, the basal ganglia helps to initiate, regulate, and refine movements, ensuring smooth and coordinated motion. Dysfunction or damage to the basal ganglia can lead to movement disorders such as Parkinson’s disease, where the coordination and control of movement are impaired.
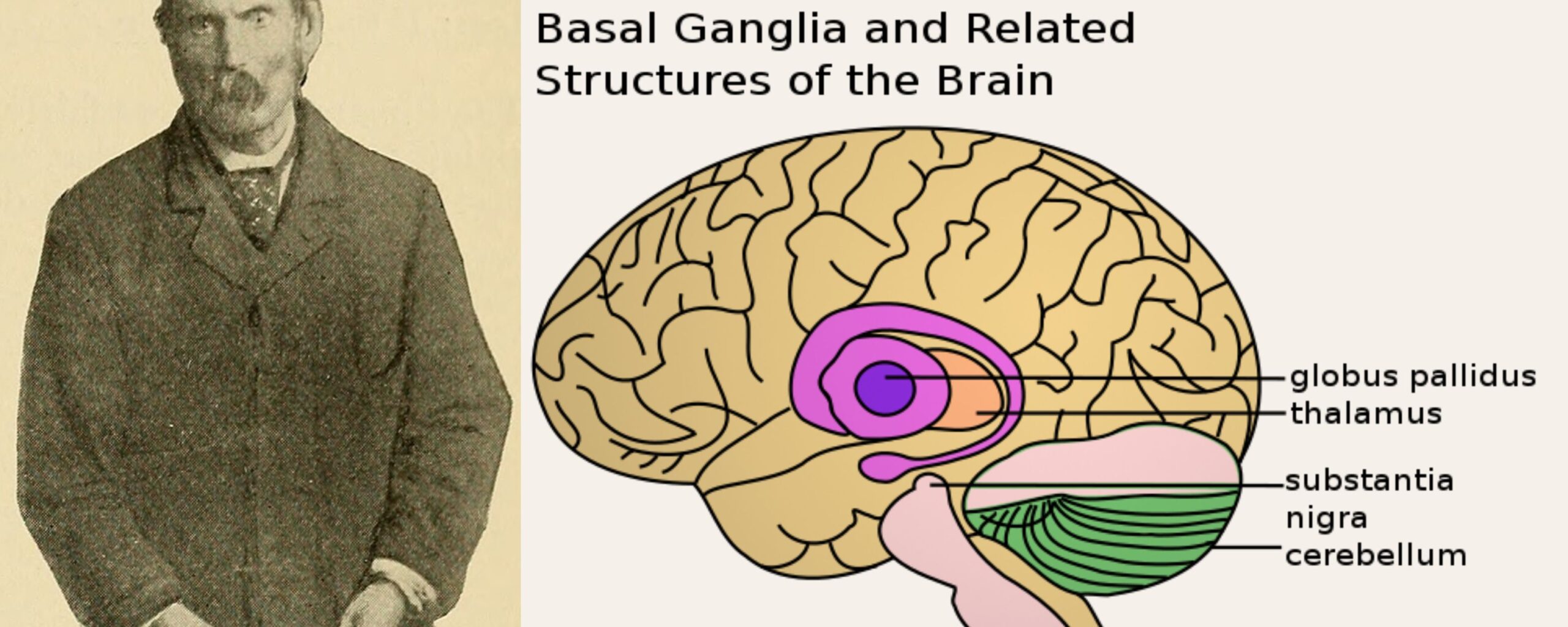
Substantia Nigra
The substantia nigra is a crucial component of the basal ganglia, tasked with the production and release of dopamine, a neurotransmitter essential for facilitating communication between nerve cells involved in movement control. When abnormal proteins accumulate in the substantia nigra, it triggers the degeneration of nerve cells, resulting in reduced dopamine production.
This dopamine deficiency impairs the ability of nerve cells to communicate effectively, disrupting the intricate network of signals required for the basal ganglia to regulate and control muscle movements. Consequently, this dysfunction leads to the motor symptoms characteristic of conditions like Parkinson’s disease.
In the later stages of Parkinson’s Disease (PD), individuals may experience non-movement-related symptoms due to a decline in the levels of another neurotransmitter called norepinephrine. Norepinephrine plays a critical role in regulating autonomic functions, including digestion, heart rate, blood pressure, and breathing. As norepinephrine levels decrease, disruptions in these autonomic functions can occur, leading to symptoms such as gastrointestinal issues, changes in heart rate and blood pressure, and breathing difficulties. These non-motor symptoms can significantly impact the overall quality of life for individuals living with PD.
Who gets Parkinson’s disease?
Parkinson’s Disease (PD) is the second most prevalent neurodegenerative disorder worldwide, trailing only Alzheimer’s Disease (AD). It predominantly affects elderly individuals, particularly males over the age of 60. However, approximately 10% of PD cases are diagnosed in individuals younger than 50 years old. Among these cases, a notable proportion have a positive family history, suggesting a genetic component in the development of the disease. This underscores the importance of genetic factors in understanding and potentially treating Parkinson’s Disease.
What are the Symptoms of Parkinson’s Disease?
Symptoms of Parkinson’s Disease can manifest in various ways, including:
- Tremors at rest, often affect one side of the body, particularly the hands or arms in the early stages.
- Symptoms worsen with stress or fatigue and diminish during sleep or deliberate movements.
- Increased muscle tone leads to stiffness or rigidity, which can impair free movement and cause pain or aches in affected muscles.
- Bradykinesia is characterized by slowness of movement and difficulty initiating activities such as getting out of a chair or performing daily tasks.
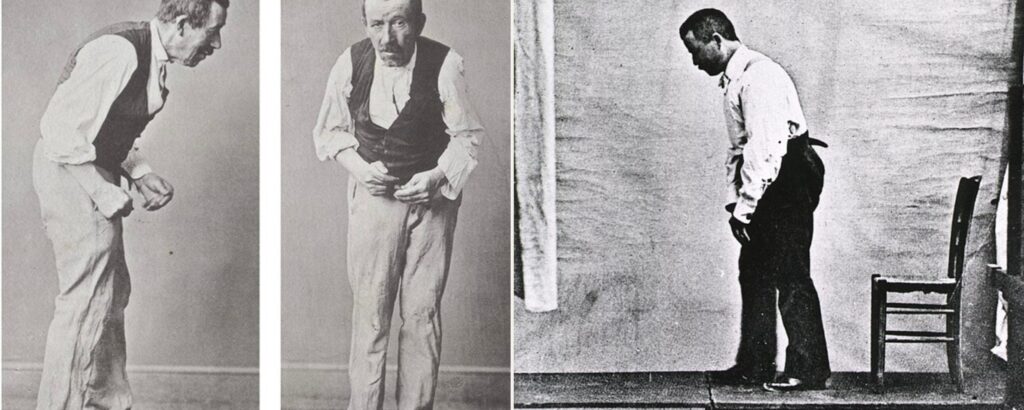
- Parkinsonian gait is characterized by unsteady balance, small quick steps, a tendency to lean forward, difficulty stopping or turning, reduced arm swinging, and a stooped posture.
- Affected fine motor skills, resulting in difficulty performing tasks like buttoning clothes or tying shoelaces.
- Micrographia, or small and shaky handwriting.
- Mask-like face or expressionless face in later stages of the disease.
- Speech issues, including speaking softly in a monotone voice or experiencing difficulty articulating words, such as stuttering.
Other symptoms may include depression, anxiety, impaired cognitive function, hallucinations, loss of smell, swallowing difficulties, constipation, urinary problems, and sleep disturbances. These additional symptoms can significantly impact the overall quality of life for individuals with Parkinson’s Disease.
What are the Stages of Parkinson’s Disease?
Parkinson’s Disease typically progresses through stages, ranging from early to mid to mid-late to advanced stages. However, it’s important to note that the symptoms and their intensity can vary significantly from person to person. No two individuals experience the exact same symptoms or progression of the disease. This variability underscores the complex nature of Parkinson’s Disease and the need for personalized approaches to treatment and care.
Early-stage Parkinson's Disease
- Mild symptoms are present.
- Daily activities are not significantly impacted.
- Changes may be noticed by family members.
- Characteristics such as lack of arm swinging, slow/small handwriting, lack of facial expression, and difficulty getting out of a chair may be observed.
Mid-stage Parkinson's Disease
- Symptoms worsen.
- Tremors, muscle stiffness, and movement problems affect both sides of the body.
- Balance issues become more evident, leading to frequent falls.
More time is required to complete tasks.
Mid-late stage Parkinson's Disease
- Walking and standing independently become difficult.
- Assistance from caregivers is required for mobility.
- The need for support with daily activities increases.
Advanced stage Parkinson's Disease
- Individuals may become wheelchair-bound or bedridden.
- Full-time caregiving assistance is necessary for daily tasks and personal care.
Management of the Parkinson’s disease
Managing Parkinson’s Disease involves addressing its symptoms and improving quality of life. Since early symptoms can resemble age-related changes or other conditions, diagnosis can be challenging. Medical history, family history, lab tests, exposure to toxins, and imaging studies like CT or MRI scans help rule out other diseases.
While there’s no cure for Parkinson’s Disease, treatment focuses on symptom management. Medications such as Levodopa/Carbidopa are commonly prescribed to alleviate motor symptoms.
Additionally, various therapies play a crucial role in managing the disease:
- Exercise: Regular physical activity helps improve mobility, balance, and flexibility. Activities like walking, swimming, and tai chi can be beneficial.
- Physical therapy: A physical therapist can design a tailored exercise program to address specific movement difficulties and improve overall mobility.
- Occupational therapy: Occupational therapists assist in maintaining independence in daily activities by teaching strategies to overcome movement challenges and recommending assistive devices.
- Speech-language therapy: Speech therapists help address speech and swallowing difficulties commonly associated with Parkinson’s Disease, improving communication and quality of life.
- Supportive therapies: Psychological support, support groups, and counseling can help individuals and their families cope with the emotional and psychological impact of Parkinson’s Disease.
By combining medication with various therapies and lifestyle modifications, individuals with Parkinson’s Disease can better manage their symptoms and maintain an active and fulfilling life.
10 Lifestyle Strategies for Enhancing Quality of Life in Parkinson’s Disease
Improving the quality of life for individuals with Parkinson’s Disease involves adopting various lifestyle strategies and making adjustments to daily routines. Here are some tips:
- Engage in regular exercise: Exercise can help improve balance, coordination, flexibility, tremors, and muscle strength. Incorporate activities like walking, swimming, yoga, or tai chi into your routine.
- Maintain a balanced diet: Consume a fiber-rich, healthy diet with plenty of fruits, vegetables, and whole grains. Stay hydrated by drinking an adequate amount of fluids throughout the day.
- Prevent falls: Take measures to prevent falls by removing hazards in the home, using assistive devices such as canes or walkers if needed, and wearing supportive footwear.
- Move slowly: Take your time when changing positions to prevent dizziness or loss of balance.
- Focus on one task at a time: Avoid multitasking and concentrate on completing one task before moving on to the next.
- Make home modifications: Install grab bars in bathrooms, add railings where necessary, and use non-skid rubber mats on slippery surfaces to reduce the risk of accidents.
- Stay socially active: Maintain social connections with friends and family, participate in community activities, and pursue hobbies and interests that bring joy and fulfilment.
- Manage stress: Practice stress-reduction techniques such as deep breathing exercises, meditation, or mindfulness to help alleviate stress and promote relaxation.
- Practice good sleep hygiene: Establish a regular sleep schedule, create a comfortable sleep environment, and avoid stimulants like caffeine or electronic devices before bedtime to improve sleep quality.
- Adhere to medication regimen: Take medications as prescribed by your healthcare provider to manage symptoms effectively and maintain overall health.
By incorporating these tips into daily life, individuals with Parkinson’s Disease can enhance their well-being and maintain a higher quality of life.
Take away
Parkinson’s Disease presents unique challenges for both patients and their caregivers. The unpredictable nature of the disease often requires constant support, love, and care. However, caregiving can also be emotionally and physically taxing, leading to stress and burnout for family members.
If you find yourself feeling overwhelmed or stressed as a caregiver, it’s important to seek support. Talking to a healthcare professional or an expert in Parkinson’s Disease can provide valuable guidance and assistance. They can offer practical advice on managing the challenges of caregiving, provide resources for support groups or respite care services, and help you develop coping strategies to better navigate the caregiving journey.
Remember, caring for someone with Parkinson’s Disease is a team effort, and it’s okay to ask for help when you need it. By prioritizing your own well-being and seeking support when necessary, you can continue to provide the best care possible for your loved one while also taking care of yourself.
TAC Desk
Editorial Process
- Medicine
- Nutrition And Diet