
Understanding Pulmonary Hypertension: Causes, Symptoms, and Treatments
Introduction
Pulmonary hypertension (PH) is a heterogeneous chronic disease that affects the arteries in the lungs and the right side of the heart, unlike systemic hypertension, which affects the entire circulatory system. PH can develop on its own or because of other health problems, and it affects people of all ages—though it is more commonly diagnosed in older adults and those with existing heart or lung disease. While it may start subtly, PH can lead to significant complications if left untreated, making early diagnosis and proper management essential.
What is Pulmonary Hypertension?
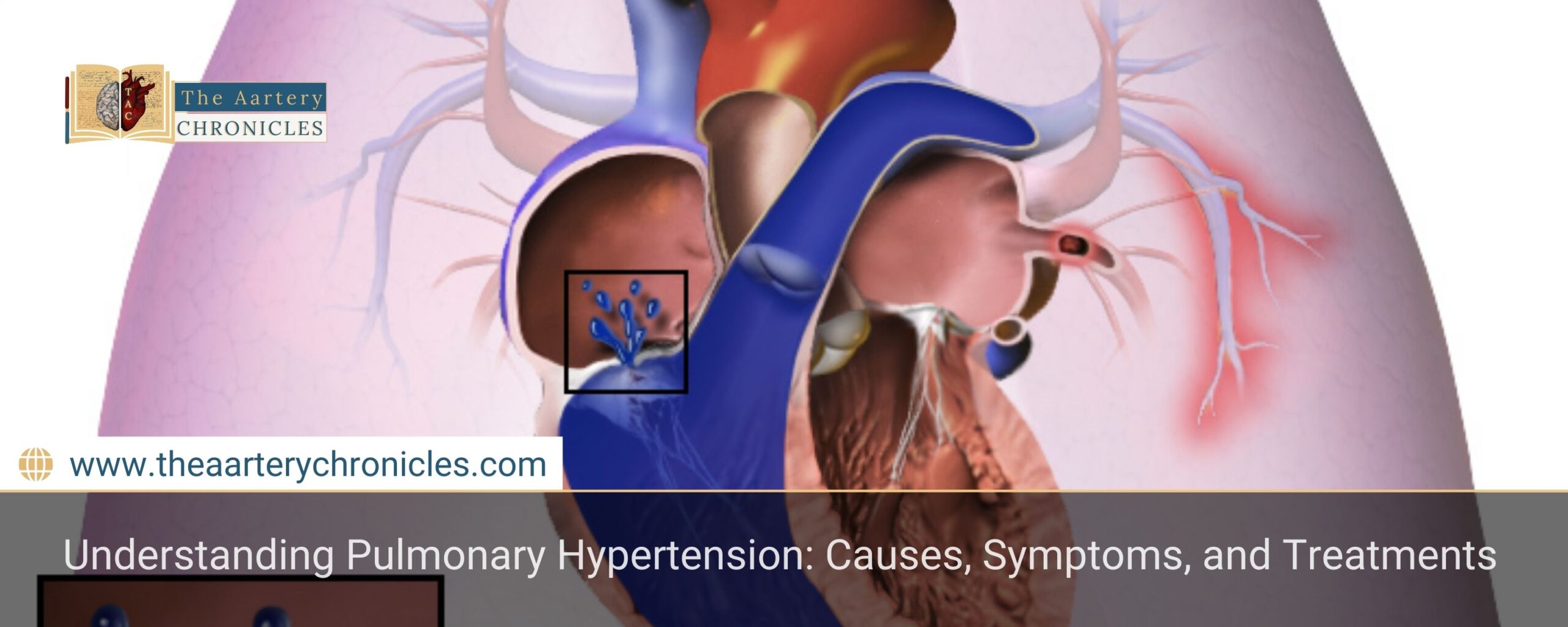
Pulmonary hypertension (PH) specifically affects the blood vessels in the lungs, causing them to narrow or become stiff. This narrowing increases resistance to blood flow, forcing the right ventricle of the heart—which pumps blood into the lungs—to work harder than normal. Over time, this extra workload can cause the right side of the heart to enlarge and weaken, ultimately leading to right heart failure, a serious and potentially life-threatening complication of PH.
This condition can stem from various underlying causes, but the hallmark feature across all forms is the increased resistance in the lung circulation. Patients with PH typically present with progressive shortness of breath (dyspnea), especially during physical exertion. As the disease advances, signs of right heart strain or right heart failure become evident, as the right ventricle works harder to pump blood through the lungs against the increased pressure.
Common Signs and Symptoms of Pulmonary Hypertension
In its early stages, pulmonary hypertension often presents with subtle, nonspecific symptoms that can easily be overlooked or mistaken for other conditions—contributing to delayed diagnosis. As PH progresses, symptoms may become more noticeable and include:
- Shortness of breath, especially during physical activity
- Fatigue
- Chest pain or tightness
- Dizziness or fainting spells
- Swelling in the ankles, leg, or abdomen
- A racing heartbeat or heart palpitations
- Decreased appetite
- Pain in the upper right side of the stomach
- Cyanosis (bluish lips or skin)
What Causes Pulmonary Hypertension?
Based on the underlying cause and mechanism driving the increased pressure in the pulmonary arteries, PH is classified into five primary groups:
A. Group 1: Pulmonary Arterial Hypertension (PAH)
Potential causes of pulmonary arterial hypertension include:
- Idiopathic PAH – Arises without a known cause.
- Heritable PAH – Resulting from genetic mutations passed through families.
- Drug-related PAH – Linked to the use of certain drugs or substances like methamphetamine.
- Congenital Heart Defects – Structural defects in the heart that are present since birth.
- Associated Conditions – Found in people with diseases like lupus, scleroderma, or liver cirrhosis
B. Group 2: Pulmonary Hypertension Due to Left-Sided Heart Disease
This is the most common type and develops when problems on the left side of the heart affect blood flow into the lungs. Common causes include:
- Left heart failure
- Aortic valve disease
- Mitral valve disease
C. Group 3: Pulmonary Hypertension Caused by Lung Conditions
This category includes diseases that affect lung function and oxygen exchange:
- Pulmonary Fibrosis – Chronic lung scarring that limits oxygen intake.
- COPD – A group of progressive lung conditions including emphysema and chronic bronchitis.
- Sleep Apnea – Interrupted breathing during sleep, affecting oxygen levels.
- Long-term High-Altitude Exposure – Especially risky for those predisposed to pulmonary hypertension.
D. Group 4: Pulmonary Hypertension from Arterial Blockages
When blockages occur in the pulmonary arteries, they can impede blood flow, resulting in elevated pressure within the lungs.
- Chronic Blood Clots – Clots that persist or keep forming in the lungs.
- Pulmonary Artery Tumors – Masses that restrict blood flow in the lung vessels.
E. Group 5: Pulmonary Hypertension Linked to Other Medical Conditions
Group 5 pulmonary hypertension is often considered the “miscellaneous” or “catch-all” category and includes PH caused by unclear or multifactorial mechanisms:
- Blood Disorders – Such as polycythemia vera or essential thrombocythemia, which increase blood thickness.
- Inflammatory Diseases – For example, sarcoidosis.
- Metabolic Disorders – like Gaucher disease or thyroid disorders.
- Chronic Kidney Disease – Long-term kidney dysfunction can also contribute.
The Five Countries Most Affected by Malaria in 2023
Category | Risk Factor |
|
|
Age | Most common between ages 30–60; risk increases with age. |
|
|
Sex | More frequently affects women than men. |
|
|
Genetics | Family history of PH or blood clots, congenital heart defects, genetic disorders. |
|
|
Lifestyle | Smoking, obesity, and use of illegal drugs (e.g., cocaine, methamphetamine). |
|
|
Environment | Long-term exposure to asbestos, high-altitude living, and certain parasitic infections. |
|
|
Medical Conditions | COPD, sleep apnea, kidney disease, autoimmune diseases, and blood-clotting disorders. |
|
|
Medications | Use of specific weight-loss, cancer, or antidepressant drugs. |
Diagnosing Pulmonary Hypertension
Doctors use a few different tests to find out if someone has pulmonary hypertension:
- Echocardiogram
- Right heart catheterization (RHC)
- Blood tests
- Chest X-rays
- CT scans
- Lung function
Treatment for Pulmonary Hypertension
While pulmonary hypertension is an incurable condition currently, there are several treatment options designed to manage symptoms and slow its progression. The choice of therapy largely depends on the root cause (based on the PH group) and the severity of the condition:
- Medications: Medications that help relieve symptoms of pulmonary hypertension include:
- Pulmonary vasodilators
- Diuretics
- Calcium channel blockers
- Endothelin receptor antagonists
- Anticoagulants
- Oxygen Therapy: Oxygen therapy is effective for those with low oxygen in blood.
- Lifestyle Changes: Incorporating lifestyle changes such as reducing salt intake, engaging in gentle exercise, and avoiding high altitudes can help manage pulmonary hypertension and may reduce the risk of worsening the condition.
- Surgery: In some cases, procedures like pulmonary endarterectomy or even lung transplantation may be necessary.
Eisenmenger Syndrome and Pulmonary Hypertension (PH)
Eisenmenger syndrome is a severe complication that arises from an uncorrected congenital heart defect—such as a hole between the heart’s chambers—which causes abnormal circulation of blood between the left and right sides of the heart.
Over time, this improper flow places increasing pressure on the lung arteries, ultimately resulting in pulmonary hypertension.
Blood flow may reverse as pulmonary hypertension worsens, enabling deoxygenated blood to travel through the body instead of via the lungs. This change in circulation causes symptoms including chest discomfort, shortness of breath, persistent weariness, and cyanosis, which gives the skin a blue color.
Eisenmenger syndrome is a late complication of uncorrected congenital heart defects and represents advanced pulmonary hypertension, often requiring lifelong care and close monitoring.
When to see a doctor?
If you are experiencing persistent shortness of breath, fatigue, or chest discomfort—especially if you have a family history of heart or lung disease—it’s important to talk to your doctor. Early diagnosis and treatment are key to managing pulmonary hypertension effectively.
If you ever have severe chest pain or trouble breathing, call 112 or go to the nearest hospital immediately.









