Listen to this article

Asthma: Pathophysiology, Diagnosis, and Management
Excerpt
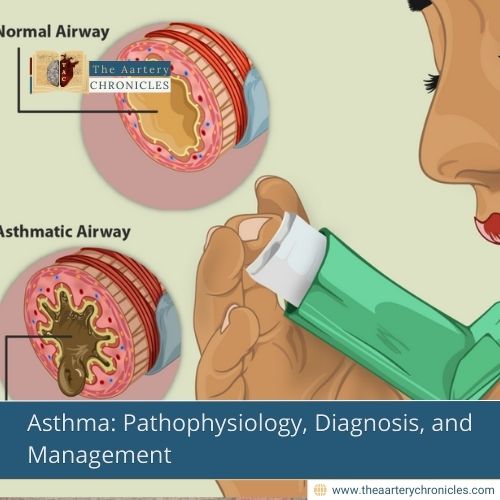
Asthma is a chronic inflammatory airway disease characterised by episodic bronchoconstriction, airway hyperresponsiveness, and mucus production. It affects millions worldwide, leading to significant morbidity. This article discusses its pathophysiology, clinical features, diagnostic approach, and management strategies, including pharmacological and non-pharmacological interventions.
ICD Codes and HCC Classification
- ICD-10 Codes:
- J45.9 (Asthma, unspecified)
- J45.2 (Mild intermittent asthma)
- J45.3 (Mild persistent asthma)
- J45.4 (Moderate persistent asthma)
- J45.5 (Severe persistent asthma)
- J45.990 (Exercise-induced bronchospasm)
- J45.991 (Cough-variant asthma)
- HCC Code: HCC 110 (Asthma and Chronic Obstructive Pulmonary Disease)
- Related Codes:
- J44.9 (Chronic obstructive pulmonary disease, unspecified)
- J46 (Status asthmaticus)
Definition
Asthma is a chronic inflammatory disease of the airways marked by episodic wheezing, dyspnea, chest tightness, and coughing, often triggered by allergens, exercise, or infections. It is characterized by reversible airway obstruction and bronchial hyperresponsiveness.
Pathology
- Inflammatory cells: Increased eosinophils, mast cells, and T-helper 2 cells.
- Airway remodelling: Goblet cell hyperplasia, subepithelial fibrosis, and hypertrophy of bronchial smooth muscle.
- Mediators: Increased levels of histamine, leukotrienes, and cytokines (IL-4, IL-5, IL-13) leading to bronchoconstriction and airway inflammation.
Types of Asthma
- Allergic (Extrinsic) Asthma: Triggered by allergens (e.g., pollen, dust mites, pet dander)
- Non-allergic (Intrinsic) Asthma: Triggered by infections, cold air, exercise, or stress
- Exercise-induced asthma (EIA): Occurs during or after physical exertion
- Occupational Asthma: Triggered by workplace irritants (e.g., chemicals, fumes)
- Aspirin-Exacerbated Respiratory Disease (AERD): Associated with NSAID sensitivity
- Cough-Variant Asthma: Persistent cough as the main symptom without classic wheezing
- Nocturnal Asthma: Symptoms worsen at night due to circadian variations in lung function
- Severe/Refractory Asthma: Persistent symptoms despite maximum treatment
Symptoms and Signs
- Episodic wheezing, dyspnoea, and chest tightness
- Cough, often worse at night or early morning
- Increased mucus production
- Symptoms triggered by allergens, cold air, exercise, or infections
Diagnosis
Pulmonary Function Tests (PFTS)
- Spirometry: FEV1/FVC <70% with >12% reversibility after bronchodilator use.
- Methacholine challenge test: Confirms hyperresponsiveness in borderline cases.
Other Diagnostic Tests
- Peak Expiratory Flow Rate (PEFR): Measures airway obstruction.
- Fractional Exhaled Nitric Oxide (Feno): Indicates eosinophilic inflammation.
- Allergy Testing: Identifies allergic triggers.
- Chest X-ray: Rules out differential diagnoses.
Differential Diagnosis
- COPD: Irreversible airflow obstruction, older age, smoking history
- Heart Failure: Basal crepitations, pulmonary oedema on imaging
- Vocal Cord Dysfunction: Stridor, normal spirometry
- Bronchiectasis: Chronic productive cough, abnormal CT findings
- Pulmonary Embolism: Sudden onset of dyspnoea, pleuritic chest pain, D-dimer elevation
Treatment
Acute Exacerbation Management
- Bronchodilators:
- Salbutamol 2.5 mg nebulised every 20 minutes or MDI 4–8 puffs every 20 minutes
- Corticosteroids:
- Prednisolone 40–60 mg PO once daily for 5 days
- IV Hydrocortisone 100 mg every 6 hours (if severe)
- Oxygen Therapy: Maintain Spo2>92%
- Magnesium Sulfate: IV 2 g over 20 minutes (for severe cases)
- Antibiotics: If ba acterial infection is suspected
Long-Term Management (Stepwise Approach)
- Step 1: Intermittent Asthma (Mild, <2 episodes per week)
- SABA (Salbutamol) PRN
- Step 2: Mild Persistent Asthma
- Low-dose ICS (Budesonide 200 mcg BID) + SABA PRN
- Step 3: Moderate Persistent Asthma
- Low-dose ICS + LABA (Budesonide/Formoterol 200/6 mcg BID)
- Step 4: Severe Persistent Asthma
- Medium/High-dose ICS + LABA ± LAMA (Tiotropium 5 mcg QD)
- Step 5: Refractory Asthma: Biologic Therapy (Omalizumab for allergic asthma, Mepolizumab for eosinophilic asthma)
Surgical Interventions
- Bronchial Thermoplasty: Reduces airway smooth muscle mass in severe asthma
Statistical Data
- Global prevalence: ~300 million people worldwide
- Asthma mortality: ~455,000 deaths annually (WHO)
- Risk factors: Genetic predisposition, environmental allergens, air pollution
Clinical Case
Patient Profile:
- A 32-year-old female with seasonal allergies presents with episodic wheezing and nighttime cough
Findings:
- Spirometry: FEV1 improved by 15% post-bronchodilator
- Feno: Elevated, suggestive of eosinophilic asthma
Treatment & Outcome:
- Started on Budesonide/Formoterol 200/6 mcg BID + Salbutamol PRN
- Symptom control was achieved within 4 weeks with improved lung function
Mnemonic for for Asthma
- ASTHMA (Symptoms)
- A: Accessory muscle use
- S: SOB (Shortness of breath)
- T: Tight chest
- H: High-pitched wheezing
- M: Mucus production
- A: Audible wheeze
- A-B-C-D for Asthma Management
- A: Albuterol (Salbutamol)
- B: Budesonide (ICS)
- C: Corticosteroids
- D: Diagnosis with Spirometry
References

Author
Dr Darshit Jagdish Patel








