Top 10 Questions Answered to Decode the Root Canal Treatment Mysteries
A thought of visiting a dentist… The atmosphere of the dental clinic, fear of pain, and the notion of someone working on their teeth can contribute to a sense of apprehension, triggering anxiety and physical discomfort.
The Artery Chronicle (TAC) is privileged to feature Dr Hardik Shah, who graciously shared his insights and expertly addressed inquiries concerning a prevalent dental procedure – Root Canal Treatment.
Dr. Hardik Shah Addresses 10 Common Patients’ Questions…
Question 1: What is a Root Canal Treatment or RCT?
Dr. Hardik: A root canal, also known as endodontic therapy, is a dental procedure performed to treat and save a tooth that is infected or severely damaged.
Here’s an overview of what happens during a root canal:
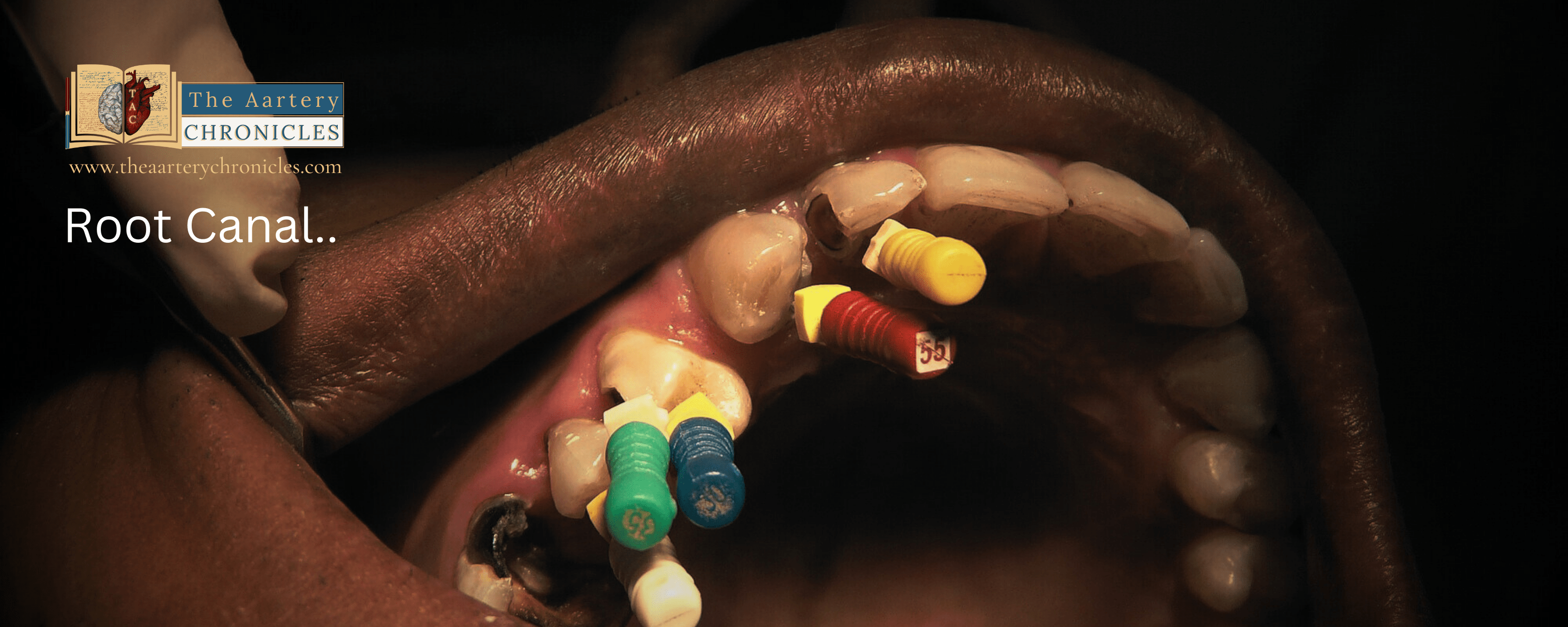
- Diagnosis: The dentist examines the tooth and uses X-rays to determine the extent of the infection or damage. If the pulp (the innermost part of the tooth) is affected, a root canal may be necessary.
- Local Anesthesia: The dentist administers local anaesthesia to numb the area around the affected tooth, ensuring the patient is comfortable during the procedure.
- Access and Cleaning: The dentist creates an opening in the crown of the tooth to access the pulp chamber and root canals. The infected or damaged pulp is removed.
- Shaping and Disinfection: The dentist cleans, shapes, and disinfects the inside of the tooth’s canals to remove any remaining bacteria or debris.
- Filling: After the canals are cleaned, they are filled with a biocompatible material, typically a rubber-like substance called gutta-percha, to seal the space.
- Restoration: In most cases, a temporary or permanent filling is placed in the access opening, and a crown may be recommended to protect and restore the tooth’s strength and function.
A successful root canal can save a tooth that might otherwise need to be extracted. It’s a common and effective procedure for relieving pain and preserving oral health.
Question 2: When and why do you need a root canal?
Dr Hardik: A root canal is typically recommended by a dentist when the innermost part of a tooth, called the pulp, becomes infected, inflamed, or damaged. This can occur for various reasons, and the need for a root canal is usually based on specific dental issues.
Common situations that may require a root canal include:
- Severe Toothache: Persistent, severe tooth pain, especially when chewing or applying pressure to the tooth, can be a sign of pulp inflammation or infection.
- Sensitivity: Increased sensitivity to hot or cold temperatures, which lingers even after the stimulus is removed, may indicate a problem with the tooth’s pulp.
- Swelling or Abscess: Swelling, a pimple-like bump on the gum, or the presence of a dental abscess can be signs of infection in the tooth’s pulp.
- Deep Decay: Advanced dental decay that has reached the pulp of the tooth can lead to infection and the need for a root canal.
- Trauma or Injury: A tooth that has been damaged due to trauma, such as a fracture or a blow to the tooth, may require a root canal to address pulp damage.
- Repeated Dental Procedures: Sometimes, a tooth that has undergone multiple dental procedures (e.g., fillings) may develop pulp issues over time and necessitate a root canal.
Dentists will perform a thorough examination, including X-rays, to diagnose the problem and recommend a root canal or other appropriate treatment to save the tooth and alleviate pain or infection. Early intervention is crucial to prevent further complications.
Question 3: How many sittings or visits will a root canal take?
Dr Hardik: The number of sittings or appointments required for a root canal procedure can vary depending on several factors, including the complexity of the case, the location of the tooth, and the individual patient’s oral health. In many cases, a standard root canal treatment can be completed in 1 to 3 appointments.
Here’s a general overview of the typical scenarios:
- Single Visit: Some straightforward root canals and non-pus-related tooth can be completed in a single visit. This is more common for front teeth (incisors and canines) with a single root.
- Two Visits: Teeth with two or more roots, such as premolars, may require two visits. The first appointment involves cleaning and shaping the canals, and the second visit is for filling and sealing the canals.
- Three or More Visits: Complex cases, especially those involving molars with multiple roots or cases with infection and abscesses, may require three or more visits for thorough treatment and to ensure the infection is completely resolved.
The dentist will assess your specific situation, and the number of sittings needed will be determined based on the severity of the infection or damage and the tooth’s location in your mouth.
Question 4: What happens if you avoid a root canal?
Dr Hardik: It is essential to undergo a recommended root canal treatment when necessary, as avoiding it can result in several negative consequences for both your oral health and overall well-being.
Here are some of the potential risks and outcomes of not getting a needed root canal:
- Persistent Pain: If you have an infected or damaged tooth, it’s likely causing you pain. Avoiding a root canal can lead to persistent and severe toothache, which can negatively impact your quality of life.
- Spread of Infection: Untreated dental infections can spread to other parts of the body, causing systemic health issues. This can lead to more extensive and costly medical treatment.
- Tooth Loss: Without a root canal, the infection or damage may progress to the point where the tooth cannot be saved. This can result in tooth extraction, which may necessitate more complex and costly dental work, such as dental implants or bridges.
- Chronic Health Issues: Prolonged oral infections can contribute to other health problems, including cardiovascular issues, diabetes, and more.
- Financial Costs: Delaying or avoiding a necessary root canal can lead to higher dental and medical costs in the long run, as more extensive treatments may be required.
- Discomfort and Reduced Quality of Life: Chronic dental pain and discomfort can have a significant negative impact on your daily life, affecting eating, speaking, and overall well-being.
Question 5: Can medication alone heal/cure root canal damage?
Dr Hardik: Medications alone cannot cure a root canal infection or damage. Root canal treatment is a dental procedure that involves the removal of the infected or damaged pulp inside a tooth and cleaning and sealing the root canals. This procedure is necessary to address the source of the infection or discomfort.
Prescribing medications before, during, or after a root canal aims to manage pain and infection. However, it’s crucial to understand that these medications are employed as part of the treatment process and do not serve as standalone cures.
Here are the typical medications used in the context of a root canal:
- Pain Management: Before the root canal procedure, a local anaesthetic is used to numb the area around the tooth, ensuring that you do not feel pain during the treatment. After the procedure, your dentist may prescribe pain relievers or recommend over-the-counter pain medications to manage any post-operative discomfort.
- Antibiotics: In cases of severe infection or the presence of an abscess, your dentist may prescribe antibiotics to help control the infection. Antibiotics, however, do not eliminate the need for the root canal procedure, as the source of the infection must be removed through the root canal itself.
The root canal procedure itself, which removes the infected pulp and seals the tooth, is the definitive treatment to address the infection or damage within the tooth. Medications are used to manage symptoms and aid in the healing process but do not cure the underlying issue.
Question 6: Is it better to get a tooth extraction or a root canal? What are the advantages of extraction over root canal?
Dr Hardik: Whether extraction of a tooth is better than a root canal depends on the specific circumstances, the condition of the tooth, and your individual oral health goals. Here are some factors to consider when deciding between a tooth extraction and a root canal:
- Tooth Preservation: A root canal procedure is performed with the goal of preserving the natural tooth structure. It involves removing the infected or damaged pulp, cleaning the canals, and sealing them. This allows you to keep your natural tooth.
- Functional and Aesthetic Benefits: Keeping your natural tooth through a root canal typically offers better chewing function and maintains the appearance of your smile.
- Severe Damage: If a tooth is severely damaged, such as in the case of extensive decay, advanced gum disease, or a serious fracture, it may not be a good candidate for a root canal. In such cases, extraction may be the only viable option.
- Cost and Simplicity: Tooth extraction is often less expensive and simpler than a root canal, especially when considering the cost of the procedure itself. However, it may lead to additional expenses for tooth replacement options, such as dental implants or bridges.
- Individual Preferences: Some people may prefer tooth extraction due to dental anxiety, the desire for a quick solution, or personal preferences.
It’s important to consult with your dentist to make an informed decision. They will evaluate the specific condition of your tooth and discuss the pros and cons of each option. Whenever possible, preserving your natural teeth is generally preferred, but there are cases where extraction is the more appropriate choice.
Question 7: What needs to be done after a root canal? What is the follow-up procedure done after a root canal treatment?
Dr Hardik: After a root canal procedure, it’s important to follow post-operative care instructions to ensure proper healing and to maintain the long-term health of the treated tooth.
Here are some things to follow up on after a root canal:
- Pain Management: You may experience some discomfort or mild pain after the procedure. For pain management which may include over-the-counter pain relievers or prescription medications.
- Avoid Chewing: It’s advisable to avoid chewing on the treated tooth until it’s fully restored with a dental crown. This helps prevent any damage to the weakened tooth structure.
- Dental Crown: In many cases, a dental crown will be recommended to protect and restore the tooth. Follow up with your dentist to schedule the placement of the crown as soon as possible.
- Oral Hygiene: Continue to maintain good oral hygiene by brushing and flossing regularly. Your dentist may provide specific instructions on caring for the treated tooth.
- Follow-Up Appointments: Attend any scheduled follow-up appointments with your dentist. These appointments are essential to ensure the tooth is healing properly and to address any concerns.
- Diet: Be cautious with your diet immediately after the root canal. Avoid very hot or very cold foods, as the tooth may be sensitive. Also, avoid hard or sticky foods that could damage the tooth.
- Pain or Swelling: If there is severe pain, swelling, or any unusual symptoms after the procedure, these could be signs of complications.
- Medications: Take any prescribed medications as directed by your dentist, including antibiotics if they were prescribed to address infection.
- Oral Care Products: Use any recommended oral care products, such as fluoride toothpaste or mouthwash, to promote the long-term health of the treated tooth.
- Regular Dental Checkups: Continue to schedule regular dental checkups and cleanings to monitor the health of your teeth and to catch any issues early.
Following these post-operative care instructions is essential for a successful recovery and the long-term success of your root canal treatment.
Question 8: Is the placement of a crown or cap necessary to place on a root canal-treated tooth?
Dr Hardik: In most cases, the placement of a crown (dental crown or cap) after a root canal is necessary and strongly recommended. A root canal procedure involves the removal of the infected or damaged pulp from the tooth, which can weaken the tooth structure.
Here’s why a crown is typically recommended after a root canal:
- Protection: After the pulp is removed, the tooth can become more brittle and susceptible to fracture. A crown provides a protective covering that strengthens the tooth and helps prevent it from breaking.
- Sealing the Tooth: The crown seals the tooth’s root canals and the access opening created during the root canal procedure, reducing the risk of reinfection.
- Restoration: A crown restores the tooth’s appearance and function. It allows you to chew, speak, and smile as you would with a natural tooth.
- Longevity: A properly placed crown can help the treated tooth last for many years or even a lifetime, which is a key goal of root canal therapy.
In some cases, a dentist may recommend other types of restorations, such as an onlay or inlay, depending on the extent of the tooth’s damage. However, a full crown is a common choice for teeth that have undergone root canals.
It’s essential to follow your dentist’s recommendations regarding the placement of a crown after a root canal to ensure the best possible outcome for your treated tooth.
Question 9: Is Re-root canal treatment good or bad?
Dr Hardik: A re-treatment of a root canal, often referred to as a “re-root canal,” may be necessary in some cases. The primary reason for re-treating a tooth that has previously undergone a root canal procedure is the persistence or recurrence of infection or discomfort.
Here are some situations that may warrant a re-root canal:
- Persistent or Recurrent Infection: In some cases, the original root canal treatment may not completely remove the source of the infection. If the infection persists or recurs, a re-root canal may be necessary to thoroughly clean and disinfect the canals.
- Undetected Canals: Some teeth have complex root canal systems, and occasionally, the dentist may miss smaller canals during the initial treatment. Re-treatment may be required to address these undetected canals.
- Deterioration: Over time, the sealant material used in the initial root canal may degrade or develop gaps, allowing bacteria to re-enter the tooth. Re-treatment can involve the removal of the old material and the re-sealing of the canals.
- New Infection: If a tooth that has had a root canal becomes re-infected, re-treatment is often needed to address the new infection source.
- Fracture or Damage: A tooth that has undergone a root canal may become fractured or damaged, leading to infection. Re-treatment may be necessary to address the new issue.
Re-root canal procedures can be more complex and challenging than initial root canals, but they are often successful in saving the tooth and addressing the issue. If you’re experiencing persistent pain or discomfort in a tooth that has previously undergone a root canal, or if a dental X-ray reveals a problem, it’s important to consult with a dentist to determine if re-treatment is necessary.
Question 10: Why there is pain even after a successful root canal procedure?
It is common to experience some degree of discomfort or pain after a root canal procedure. This pain is typically mild to moderate and can be managed with over-the-counter pain medications, as recommended by your dentist. The following factors can contribute to post-root canal pain:
- Inflammation: The tissues around the tooth may still be inflamed following the procedure. This can lead to some discomfort, which should gradually subside over a few days.
- Tenderness: The tooth and surrounding tissues may be tender due to the treatment. This tenderness can result in mild pain or discomfort.
- Infection Resolution: If there is a severe infection before the root canal, it may take time for the body to completely heal and the pain to fully subside.
- Temporary Filling: In some cases, a temporary filling is placed after the root canal procedure. This filling is later replaced with a permanent restoration, like a dental crown. The temporary filling may not provide the same level of protection and comfort as the permanent restoration.
- Individual Variability: Each person’s pain threshold and healing process are unique, so the level of discomfort can vary from person to person.
If you experience pain after a root canal, it’s generally manageable with over-the-counter pain relievers like ibuprofen, diclofenac etc. However, if the pain is severe, increasing, or not improving, or if you notice swelling or other concerning symptoms, it’s important to contact your dentist promptly.

Author: Dr. Hardik Shah,
BDS, Implantologist
- Health Updates
- Medicine
- Nutrition And Diet
- Biotechnology