Beyond the Taboo: Psychedelic Therapy’s Role in Mental Health
Summary: Psychedelic therapy, once stigmatized, is now at the forefront of mental health research. Substances like psilocybin, MDMA, ketamine, and LSD are showing promise in treating depression, PTSD, and addiction, with growing clinical evidence and cautious optimism shaping their future role in psychiatry.
Introduction
Once considered a taboo and marginalised area of psychiatry, psychedelic therapy has now emerged as a leading focus in cutting-edge mental health research. With increasing clinical trials and FDA-backed studies, substances like psilocybin (magic mushrooms), MDMA, ketamine, and LSD are showing powerful potential in treating mental health disorders such as depression, PTSD, and addiction. After decades of legal restrictions and stigma, psychedelic therapy is being re-evaluated with scientific rigour and cautious optimism.
A Brief History of Psychedelic Treatment
The Evolution of Psychedelic Research
Clinical research into psychedelics began in the mid-20th century, focusing initially on substances like LSD (lysergic acid diethylamide) and psilocybin, the active ingredient in what are commonly known as “magic mushrooms.” Researchers like Humphrey Osmond and Abram Hoffer began experimenting with LSD in 1951, hypothesising that it could unlock heightened self-awareness with significant therapeutic promise.
Initial studies highlighted psychedelics’ profound impact on consciousness and suggested potential applications in treating mental health conditions like depression, anxiety, and addiction.
The 1960s: A Shift in Perception
The 1960s represented a pivotal moment when psychedelics became closely associated with the counterculture and anti-establishment movements of the time. LSD, often distributed via sugar cubes, gained popularity among the public, especially within the growing hippy subculture. This widespread use sparked concern, and by the mid-1960s, psychedelics were increasingly viewed as substances of abuse.
In response, the British government banned LSD in 1966, followed by the United States in 1968, largely due to its perceived link to social unrest and anti-war activism. Due to increasing recreational use, political backlash, and cultural fears, most psychedelics were criminalized under the Controlled Substances Act of 1970 in the United States.
The 2000s: A Scientific Reawakening
Toward the end of the 20th century and into the early 2000s, interest in psychedelics experienced a significant revival. The “psychedelic renaissance” began in the 2000s when regulatory bodies like the FDA started approving limited studies under strict supervision.
Research expanded to include the treatment of addiction, with notable results. For example, a 2014 study by the Johns Hopkins Center for Psychedelic and Consciousness Research found that 80% of smokers given psilocybin were able to quit, compared to just 35% of those using traditional nicotine replacement therapies.
Further studies explored the use of psychedelics for depression and anxiety, particularly in patients facing life-threatening illnesses. In 2016, a landmark trial reported that a single dose of psilocybin provided substantial relief from cancer-related anxiety and depression for up to six months.
The 2020s and Beyond: A Promising Future
Today, psychedelic research is accelerating rapidly and institutions such as Johns Hopkins University, MAPS (Multidisciplinary Association for Psychedelic Studies), and Imperial College London are leading research efforts.
Increased funding, improved clinical methodologies, and broader public and regulatory acceptance are paving the way for these substances to become part of mainstream mental healthcare.
How Psychedelic Therapy Works
Over the past 20 years, a growing number of studies have examined the effects of various psychedelic compounds on mood disorders, anxiety, and substance use disorders, with encouraging results showing both effectiveness and good safety profiles in controlled research environments. While it’s still not fully understood how psychedelics can address such a wide range of conditions, several explanatory theories are currently being explored.
Functional neuroimaging has revealed that psychedelics may temporarily disrupt the default mode network—a set of brain regions associated with self-focused thinking and introspection. This network tends to be hyperactive in many psychiatric and substance use disorders. By interrupting its activity, psychedelics may allow the brain to reset and adopt more flexible thinking patterns, potentially supporting healthier behaviors and coping strategies.
On a neurochemical level, psychedelics appear to enhance neuroplasticity—the brain’s capacity to reorganize itself and form new connections—for an extended period after the drug’s immediate effects wear off. This heightened plasticity may help patients develop new insights, adopt different perspectives, and make enduring changes in behavior and thought.
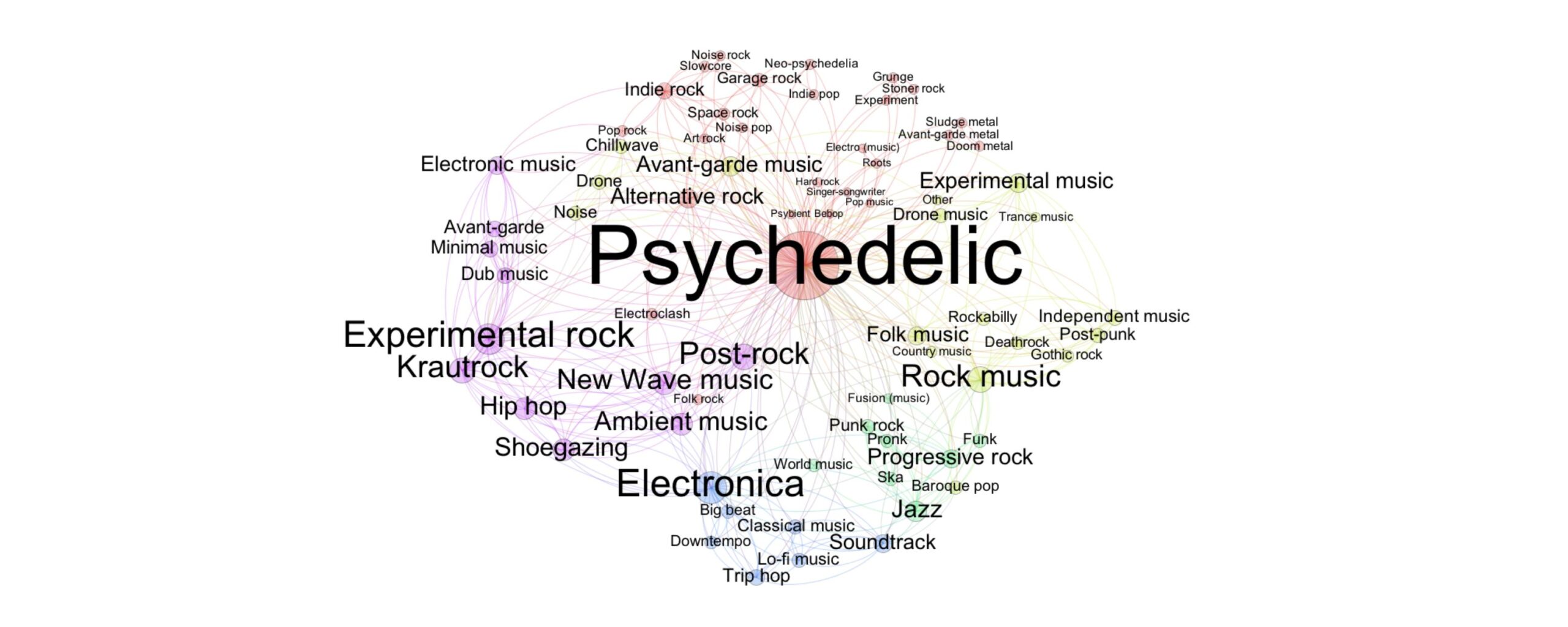
Psychedelic Drugs
Psychedelic substances can deeply influence perception, thinking, mood, emotions, social connection, and one’s sense of self or meaning. What sets them apart is their ability to dramatically shift consciousness without causing delirium. Common subjective effects include changes in visual perception, hallucinations or pseudohallucinations, a heightened sense of connection, and mystical-type experiences—often described as feelings of unity, timelessness, and profound emotional or spiritual insight. Unlike many other substances, the effects of psychedelics are especially shaped by “set and setting,” meaning the individual’s mental state and the surrounding physical and social environment during use.
Key Substances in Psychedelic Therapy
1. Psilocybin
A major study found that a single dose of psilocybin, with psychological support, led to rapid and lasting relief from depression for up to 12 weeks. COMP360, a psychedelic compound derived from magic mushrooms, demonstrated encouraging results in a phase 2 clinical trial for treatment-resistant depression. Dr. David Hellerstein noted the findings could mark a significant step forward in psychiatric treatment if approved.
2. MDMA (Ecstasy)
MDMA promotes empathy and emotional openness and is currently in late-stage clinical trials for the treatment of Post-Traumatic Stress Disorder (PTSD). It is expected to receive FDA approval for this use in the near future.
3. Ketamine
Esketamine (Spravato), a nasal spray version of ketamine, was approved by the FDA in 2019 for individuals with treatment-resistant depression. It must be administered under the supervision of a healthcare provider in a certified clinic, where patients are monitored after each dose. Ketamine is not considered a first-line treatment; it is typically used when other, more traditional therapies have failed. While it does not cure depression, it can provide temporary relief from symptoms.
Current Research and Clinical Trials
- The Johns Hopkins Center for Psychedelic and Consciousness Research is actively studying the therapeutic potential of psychedelics in individuals facing a wide range of complex conditions. These include addiction (such as smoking, alcohol, and substance use), existential distress linked to life-threatening illnesses, major depressive disorder, anorexia nervosa, post-treatment Lyme disease, depression related to Alzheimer’s disease, and obsessive-compulsive disorder (OCD).
- MAPS has completed Phase 3 trials on MDMA-assisted therapy for PTSD with significant success rates—over 65% of participants no longer met PTSD criteria after treatment.
- In the UK, researchers are exploring psilocybin-assisted therapy for anorexia nervosa, a disorder with limited treatment options.
Ethical and Regulatory Considerations
Despite promising results, psychedelic therapy raises complex ethical and legal questions:
- Access and Equity: Will these treatments be affordable and accessible to people across different socioeconomic and cultural backgrounds, or will they remain limited to privileged groups?
- Safety and Oversight: Ensuring patient safety requires strict protocols for screening, professional supervision during sessions, and structured post-treatment integration to support long-term outcomes.
- Potential for Abuse: As interest grows, so does the risk of misuse or self-medication without clinical guidance, which could lead to psychological harm or undermine public trust in legitimate therapy.
- Commercialization: There are concerns that large pharmaceutical companies may commercialize psychedelics in ways that prioritize profit over patient well-being, distorting their original therapeutic or cultural significance.
Conclusion
Psychedelic therapy is reshaping our understanding of mental health treatment. While it’s not a magic bullet, for many people—especially those for whom traditional medications have failed—it offers a radically new pathway to healing. As science catches up with centuries of indigenous knowledge and underground use, the coming years may see psychedelics become not just accepted, but essential tools in modern psychiatry.
- About — Center for Psychedelic & Consciousness Research
- Psychedelic-assisted therapy: An overview for the internist | Cleveland Clinic Journal of Medicine
- Ketamine for treatment-resistant depression: When and where is it safe? - Harvard Health
- MDMA enhances emotional empathy and prosocial behavior - PMC
- Psilocybin Found to Rapidly Improve Depression in Clinical Trial | Columbia University Department of Psychiatry
- The History of Psychedelics - MAC Clinical Research
- MAPS PBC Announces Publication of Results from Confirmatory Phase 3 "MAPP2" Trial of MDMA-Assisted Therapy for PTSD in Nature Medicine
- New multi-centre clinical trial to investigate psilocybin therapy in anorexia nervosa
- Dr Anjali Singh
- Medicine and Diseases
- 3 September 2025
- 11:00
Reviewed by Dr Aarti Nehra (MBBS, MMST)