
All About Varicose Veins: A Complete Guide
Introduction
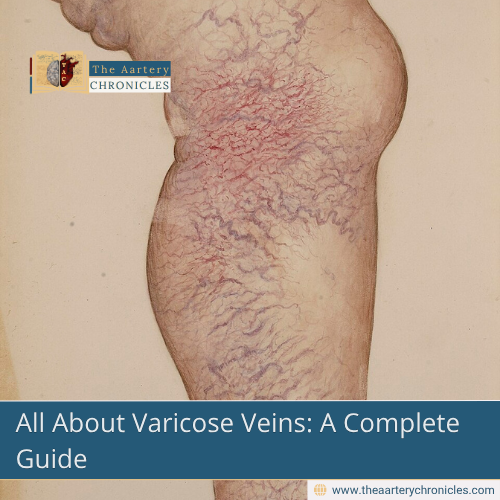
Varicose veins are a common condition that affects the veins, most often in the legs and feet. These veins become enlarged, twisted, and visible under the surface of the skin. Although varicose veins are frequently viewed as a cosmetic concern, they can cause discomfort, pain, and potentially lead to more serious health problems if not properly managed.
What Are Varicose Veins?
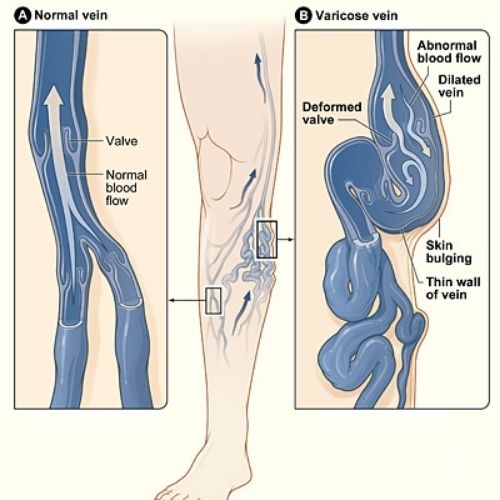
Varicose veins develop when the valves inside the veins stop working properly. Normally, these one-way valves help direct blood toward the heart. However, malfunctioning of valves in the leg veins results in backward blood flow and pooling in the veins. These veins often appear dark blue or purple and may look swollen or bulging, resembling cords running just beneath the skin.
What Causes Varicose Veins?
Increased pressure in the lower body veins is one of the main contributors to varicose veins. This pressure can result from standing or sitting for extended periods. Other contributing factors include:
- Aging: As we age, veins lose elasticity and valves may weaken.
- Hereditary: This condition can be inherited if it runs in the family.
- Gender: Women are at a higher risk of developing varicose veins, largely because hormonal fluctuations during pregnancy, menstruation, and menopause can affect vein health.
- Pregnancy: The increase in blood volume and hormone levels during pregnancy can enlarge veins.
- Obesity: Excess body weight adds pressure to veins.
- Lack of movement: A sedentary lifestyle can impair circulation and worsen vein function.
Signs and Symptoms of Varicose Veins
Varicose veins are not always painful, but they may cause a range of symptoms, especially as the condition progresses. Common signs and symptoms include:
- A heavy or aching sensation in the legs
- Burning, throbbing, or cramping in the lower limbs
- Swelling in the ankles or feet
- Itchy skin or a rash near the affected veins
- Skin discoloration or inflammation
- Visible, bulging veins
Prompt medical care is required in severe cases where varicose veins can result in ulcers, bleeding, or blood clots.
Complications of Varicose Veins
Though varicose veins are often harmless, they can sometimes lead to complications, particularly if left untreated. These may include:
- Blood Clots (Superficial Thrombophlebitis): Sometimes, varicose veins become inflamed due to a clot forming within the vein which causes the resulting vein to become warm, hard, and painful to the touch.
- Deep Vein Thrombosis (DVT): In rare cases, blood clots can form in deeper veins, posing a serious risk if the clot travels to the lungs (pulmonary embolism). Signs include swelling, redness, and pain in the leg.
- Pulmonary embolism: Pulmonary embolism occurs when a blood clot, often originating from deep vein thrombosis (DVT), travels to the lungs. This serious condition can be life-threatening and demands urgent medical attention
- Chronic Venous Insufficiency: This occurs when the veins are unable to pump enough blood back to the heart, leading to long-term swelling, skin changes, and ulcers.
When to See a Doctor
Although varicose veins are often harmless, it’s important to consult a doctor if you experience persistent pain, swelling, skin changes, or sores near the veins. A healthcare provider can diagnose varicose veins through a physical examination and may use ultrasound imaging to assess blood flow and rule out other conditions.
Treatment Options
The treatment of varicose veins depends on the severity of the condition and the patient’s overall health. Often, making simple lifestyle adjustments can ease symptoms and help stop the condition from progressing.
Lifestyle Modifications
- Regular physical activity, such as walking or swimming
- Elevating the legs when resting
- Wearing compression stockings to improve blood flow
- Maintaining a healthy weight
- Avoiding prolonged periods of sitting or standing
Medical Treatments
If lifestyle changes are not enough, several medical procedures are available:
- Sclerotherapy: In this procedure, a chemical is injected into the vein, making the vein walls seal shut, form scar tissue, and slowly disappear over time.
- Laser Therapy: Laser light is used to close off small varicose veins or spider veins.
- Endovenous Ablation Therapy: A catheter delivers radiofrequency or laser energy to seal the vein shut.
- Ambulatory Phlebectomy: Small varicose veins are removed through tiny incisions in the skin.
- Vein Ligation and Stripping: Larger veins are tied off and removed surgically.
These procedures are generally safe, minimally invasive, and offer effective relief from symptoms.
Preventing Varicose Veins
While not all cases can be prevented, certain habits can reduce the risk of developing varicose veins or slow their progression:
- Stay active and exercise regularly
- Avoid wearing tight clothing and high-heeled shoes, as they can hinder proper blood circulation
- Elevate your legs when possible
- Maintain a healthy weight and diet
- Wear compression garments if recommended by a healthcare provider
Conclusion
Varicose veins are a common condition that can range from a mild cosmetic issue to a more serious health concern. Understanding the causes and recognizing the symptoms early can help in managing the condition effectively. With proper lifestyle changes and, when needed, medical treatment, most people can find relief and improve their quality of life. If you are experiencing symptoms or are concerned about the appearance of your veins, consult with a healthcare professional for a proper evaluation and treatment plan.
- Dr Anjali Singh
- Medicine and Diseases
- 4 August 2025
- 11:00
Reviewed by Dr Aarti Nehra (MBBS, MMST)








