Why Recurrent UTIs Remain an Ignored Concern in Women’s Health
Summary:
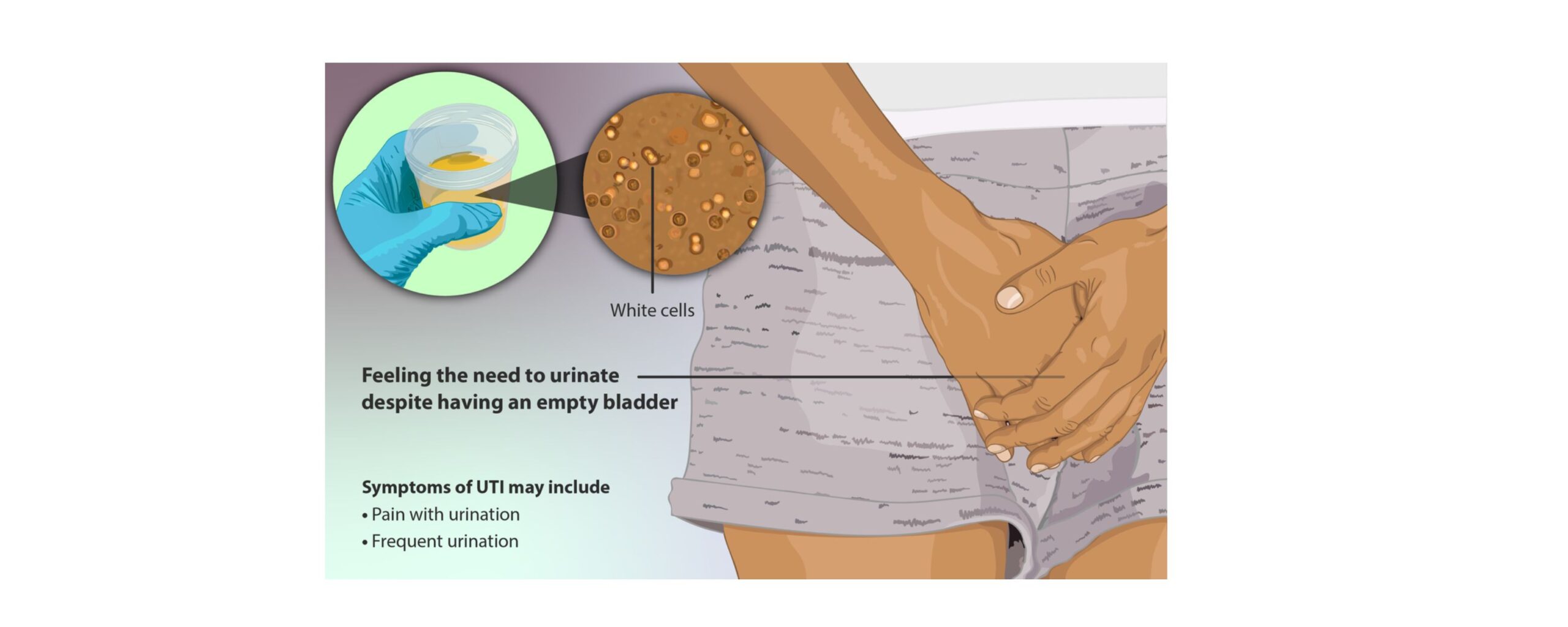
Understanding UTI
Urinary tract infections (UTIs) are among the most common infections affecting women, yet conversations about them remain hidden due to unnecessary taboo and shame. Clinical inattention, fragmented care pathways, and a lack of sympathetic, evidence-based strategies add to the suffering and humiliation of repeated UTIs for many women worldwide. This silence does not contribute to society’s well-being. Instead, it causes pain, elevates financial and healthcare system burdens, and hinders development toward health equity.
Acknowledging a Common Burden
About 30% to 40% of women experience recurrent UTIs, which are defined as two or more infections in six months or three or more in a year, at some point during their lifetimes. These infections do not reflect bad hygiene or the outcome of personal failure to maintain it. Rather, they are the result of a mix of biological, behavioural, and structural risk variables, one of them most often being the presence of Escherichia coli germs moving from the intestinal tract.
Approximately 50 to 60 percent of women will experience at least one urinary tract infection in their lifetime. Of these, nearly one in four will have a recurrence within six months, and for some, the cycle of recurrent infections continues year after year. The overall lifetime risk is significant.
Systemic Health and Equity Issues
Although anybody can be impacted, institutional problems sometimes increase the load amongst particular groups:
- Age-related risk: Both younger women, owing to anatomy, and postmenopausal women, because of hormonal changes, are disproportionately at risk. Post-menopause vaginal pH alterations help bacteria to grow rapidly, and the decrease in protective Lactobacillus species increases the vulnerability to infection.
- Comorbidities: Women with diabetes, pelvic floor issues, urinary retention, or kidney stones are more prone to recurrent UTIs.
- Socioeconomic and racial disparities: People with limited access to healthcare, health education, or adequate sanitation facilities in marginalized areas face greater health risks and reduced access to appropriate care.
With healthcare costs estimated in the billions, the societal and economic consequences of recurring UTIs are significant. For women dealing with frequent infections, the experience goes much beyond symptoms: pain, missed work, sexual dissatisfaction, and declining mental health are rather typical consequences.
Breaking down Barriers: Why the silence?
Talking about urinary health is still taboo despite the enormous weight. Women too frequently experience condescending assumptions about behaviour or cleanliness. Furthermore, perpetuating silence constrains research funding, inadequate public health communication, and a paucity of female practitioners in urology. This gendered bias in medicine can cause delayed diagnosis, needless pain, and a lack of patient-centred care.
Reframing Prevention: Facts, Not Blame
Stopping recurring UTIs calls for a change from antiquated, blame-based techniques to all-encompassing, equality-oriented solutions:
Individual-Level Solutions
Scientific evidence supports behavioural modifications and self-care interventions:
- Hydration: More fluid intake aids in cleansing the urinary tract of bacteria.
- Urination Habits: Not postponing urination and voiding after sex helps to decrease bacterial presence.
- Personal Hygiene: Wiping front-to-back and mild, scent-free products avoids bacterial translocation.
- Clothing options: Avoiding tight-fitting clothing and wearing breathable cotton underwear reduces risk.
- Postmenopausal treatments: Some women may restore protective flora with vaginal oestrogen treatment.
Community and Systemic Solutions
- Access to care: Universal, stigma-free basic care services for early diagnosis and patient education are absolutely necessary.
- Shared Decision-Making: Women claim to be more satisfied and show better results when they are active partners in decisions, especially about recurring treatments and substitutes for antibiotics.
- Antibiotic Monitoring: It is essential to use antibiotics cautiously, as their overuse contributes to the rise of resistant bacteria. Current strategies include patient-initiated treatment plans, postcoital prophylaxis for select high-risk groups, and increasing research into non-antibiotic alternatives.
Non-Antibiotic Approaches and the Research Imperative
Research on probiotics, cranberry products, vaccines, and changes to the vaginal and urinary microbiome has gained momentum. Such techniques aim to empower women and lower both healthcare expenses and the threat of antimicrobial resistance.
Listening to Lived Experience
The most frequent wish for women with recurring UTIs is simply to be heard and treated seriously. Qualitative research indicates that repeated rejection or fragmented care aggravates the misery, hence fostering mistrust and avoidance of the health system. Training healthcare providers in both scientific best practices and compassion is required to solve this.
Towards Open Conversation and Health Equality
Strong public health efforts are needed for the future. Breaking taboos, highlighting the voices of those impacted, and guaranteeing access to evidence-based prevention and treatment independent of age, socioeconomic level, or geographical location starts with a conversation to destigmatize recurrent UTIs. Equal attention to this “invisible” pandemic will change women’s health, raise living standards, and promote a fairer health system.
Let’s break the silence. Women’s urinary health is public health—worthy of our voice, our investment, and our continuous inquiry.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3749018/
- https://www.aafp.org/pubs/afp/issues/2016/0401/p560.pdf
- https://academic.oup.com/jid/article/230/5/e1101/7701247
- https://www.sciencedirect.com/science/article/pii/S1879522614000037
- https://www.frontiersin.org/journals/urology/articles/10.3389/fruro.2023.1264299/full
- https://www.sciencedirect.com/science/article/abs/pii/S0263931923000418
- https://www.ncbi.nlm.nih.gov/books/NBK557479/
- https://www.mdpi.com/2036-7481/16/3/66
- https://pubmed.ncbi.nlm.nih.gov/20842992/
- https://www.mdpi.com/2392-7674/12/1/5
- Dr Yashvi Singh
- Medicine and Diseases,Public Health
- 1 August 2025
- 11:00
Reviewed by Dr Aarti Nehra (MBBS, MMST), & Dr Darshit Patel (MBBS)








