Bronchitis: All You Need To Know about it
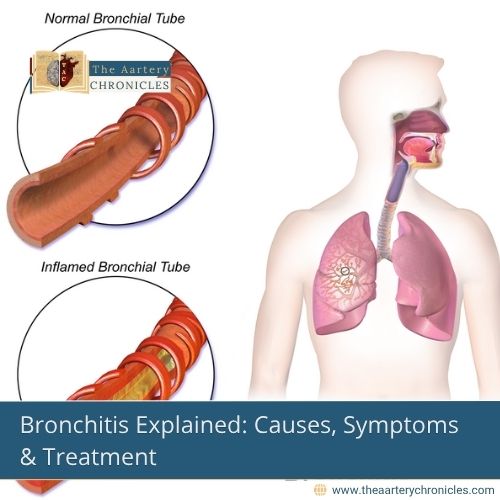
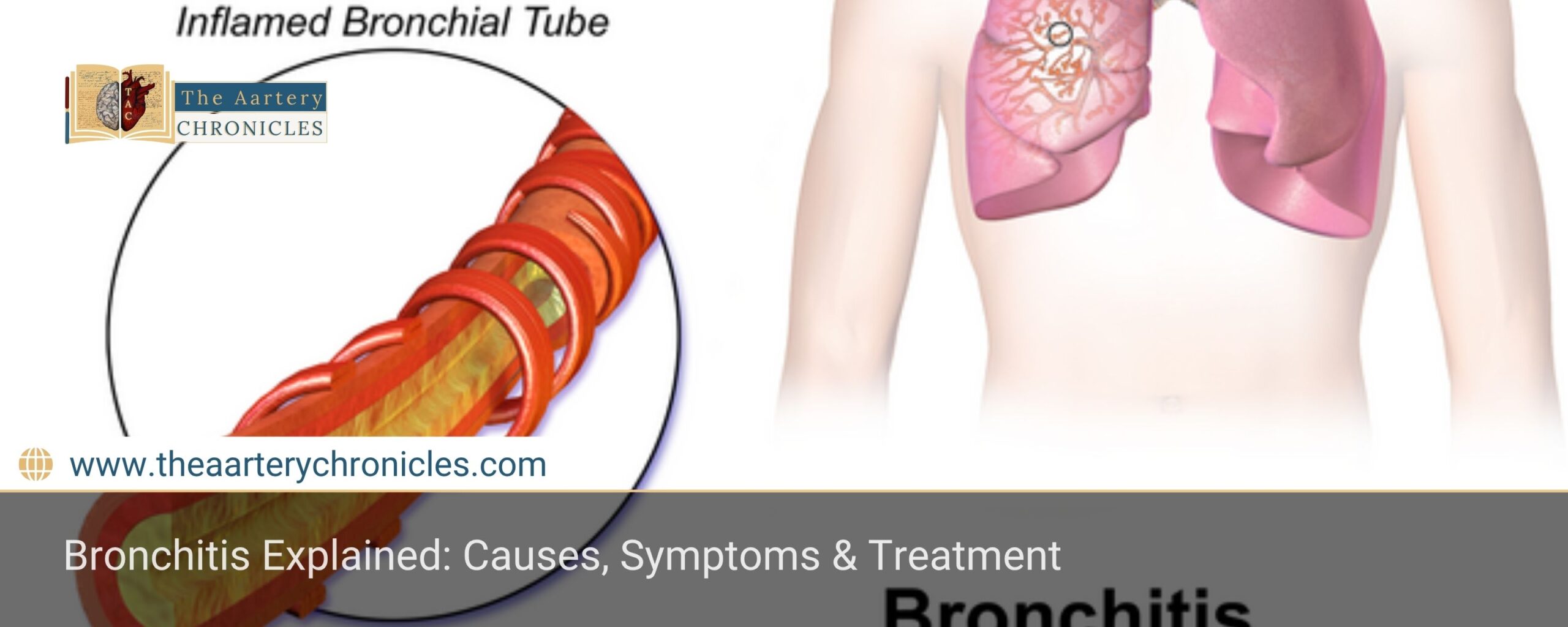
Bronchitis is an inflammation of the bronchial tubes, typically caused by viral or bacterial infections, environmental factors, or chronic lung diseases. It manifests as a persistent cough, mucus production, and airway irritation. While acute bronchitis often resolves with supportive care, chronic bronchitis, a form of chronic obstructive pulmonary disease (COPD), requires long-term management. This article provides an in-depth review of bronchitis, including its pathology, symptoms, diagnostic approach, treatment regimens, and clinical case studies
ICD Codes and HCC Classification of Bronchitis
ICD-10 Codes:
- J20.9 – Acute bronchitis, unspecified
- J20.8 – Acute bronchitis due to other specified organisms
- J42 – Unspecified chronic bronchitis
- J44.0 – COPD with an acute lower respiratory infection
HCC Code: HCC 111 (Chronic Obstructive Pulmonary Disease)
Definition of Bronchitis
Bronchitis is the inflammation of the bronchial mucosa, leading to mucus hypersecretion and airway obstruction. It is classified into:
- Acute Bronchitis – A self-limiting condition, primarily viral, lasting up to 3 weeks.
- Chronic Bronchitis – Defined as a productive cough lasting at least 3 months per year for 2 consecutive years, often associated with smoking and environmental pollutants.
Pathology of Bronchitis
Bronchitis involves distinct pathological changes depending on whether it’s acute or chronic, primarily affecting the bronchial lining and mucus production.
Acute Bronchitis
Viral infection leads to:
- Inflammation
- Bronchial oedema
- Increased mucus production
Common viral pathogens: Influenza virus, Respiratory Syncytial Virus (RSV), Rhinovirus, Coronavirus.
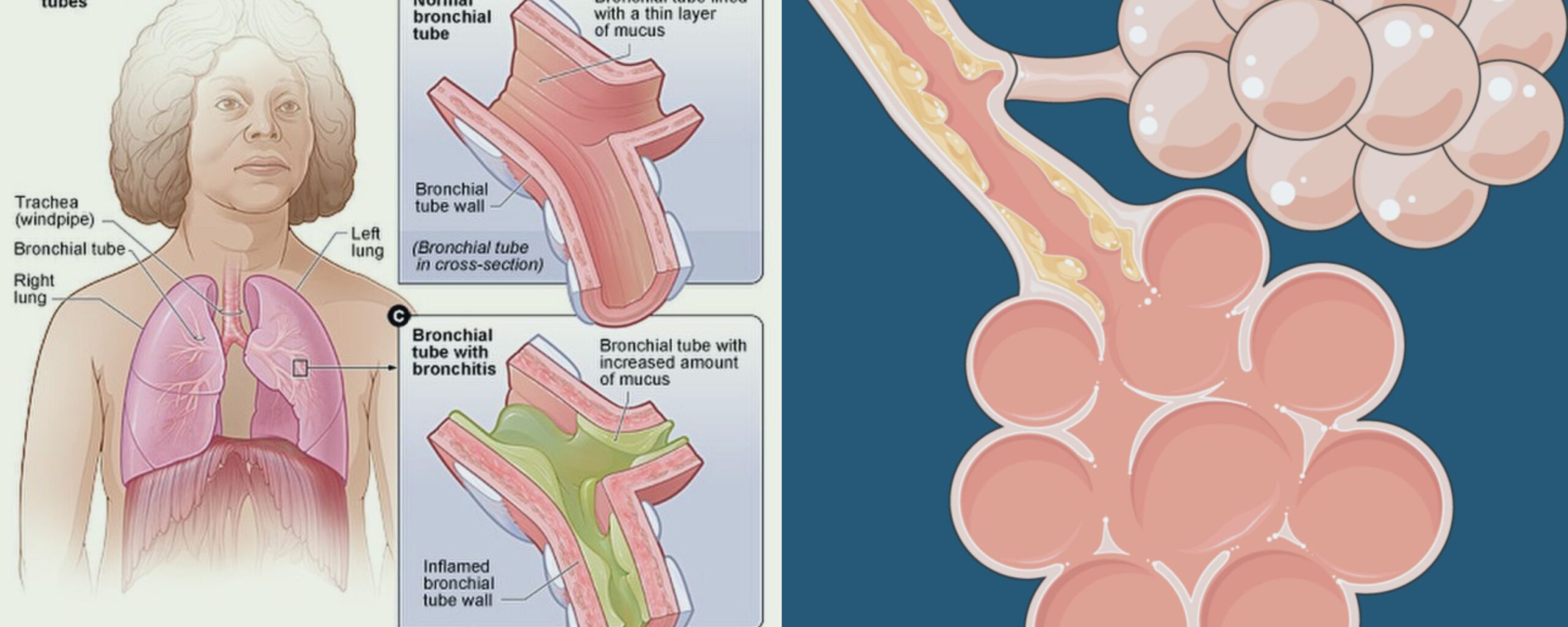
Chronic Bronchitis
Persistent irritation causes
- Hypertrophy of mucus glands
- Goblet cell hyperplasia
- Airway narrowing
Triggering factors: Often triggered by
- Smoking
- Air pollution
- Occupational dust exposure
Aetiology and Risk Factors of Bronchitis
Bronchitis can arise from infectious agents or non-infectious triggers, with viral infections being the most common cause, followed by environmental and chronic health factors
Infectious Causes:
- Viral (90% of cases): Influenza, RSV, Adenovirus
- Bacterial (rare): Mycoplasma pneumoniae, Bordetella pertussis, Chlamydia pneumoniae
Non-Infectious Causes:
- Environmental Irritants: Smoking, air pollution, allergens
- Chronic Conditions: COPD, GERD, asthma
- Immunocompromised States: HIV/AIDS, chemotherapy
Symptoms and Signs of Bronchitis
Bronchitis typically presents with a persistent cough and respiratory discomfort, with symptom patterns varying between acute and chronic forms.
Common Symptoms of Bronchitis
- Persistent cough (dry or productive)
- Sputum production (clear, yellow, or green)
- Wheezing or shortness of breath
- Chest discomfort or tightness
- Fatigue and mild fever
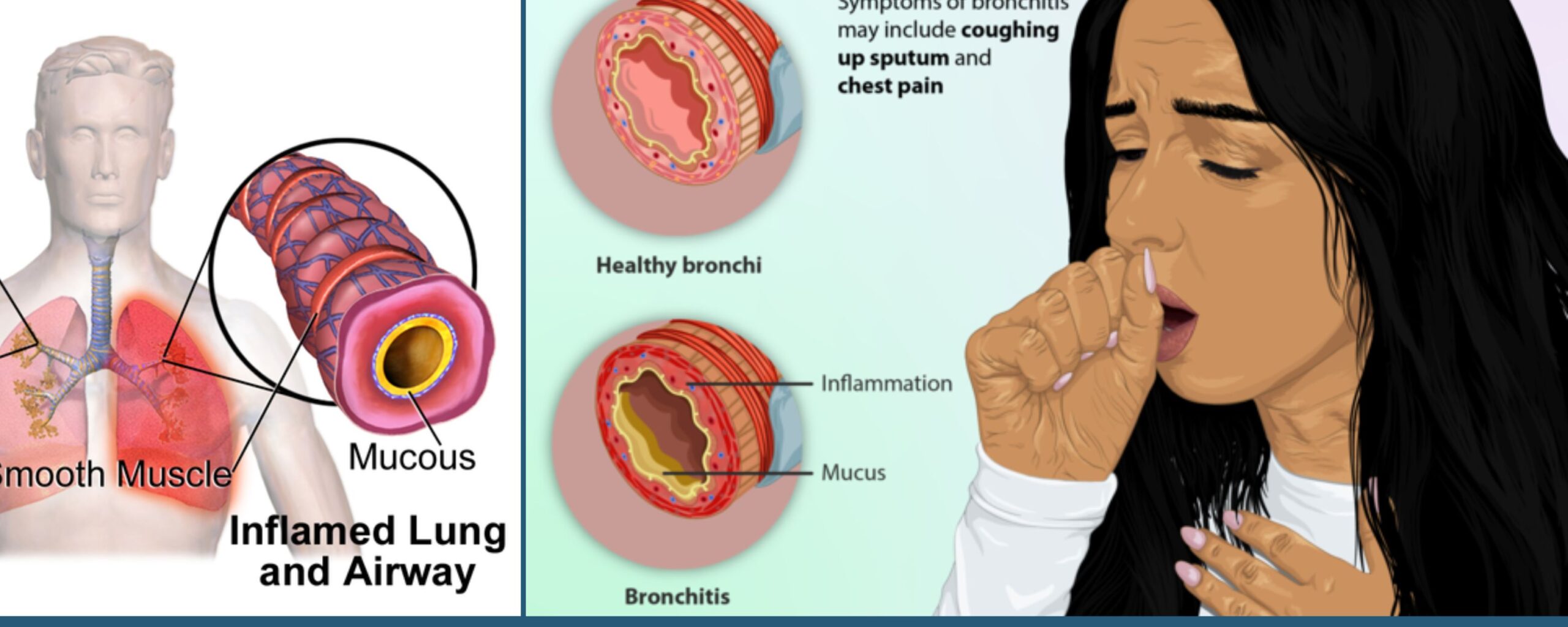
Acute Bronchitis Signs:
- Low-grade fever
- Nasal congestion and sore throat
- Diffuse wheezing or rhonchi
Chronic Bronchitis Signs:
- Persistent, worsening cough
- Frequent respiratory infections
- Cyanosis (in severe cases)
When to See a Doctor
Seeking medical attention is advised when experiencing:
- Severe or Prolonged Symptoms:
- Cough lasting more than 3 weeks
- High fever (>38.5°C) that does not subside
- Respiratory Distress:
- Difficulty breathing, shortness of breath at rest
- Wheezing not relieved by usual medications
- Hemoptysis (Coughing up Blood):
This may indicate tuberculosis, lung cancer, or severe bronchitis - Underlying Health Conditions:
Patients with asthma, COPD, heart disease, or diabetes should seek early medical evaluation - Altered Mental Status:
Confusion, drowsiness, or difficulty staying awake (especially in elderly patients) - Recurrent Bronchitis Episodes:
More than 3 episodes per year may suggest chronic bronchitis or undiagnosed COPD
Diagnosis of Bronchitis
Diagnosing bronchitis involves a combination of clinical evaluation, targeted lab tests, and imaging to differentiate between acute and chronic forms and rule out other conditions.
Clinical Evaluation
A thorough clinical evaluation is the first step in diagnosing bronchitis and involves gathering patient history and performing a physical examination to identify characteristic signs:
History Taking:
Understanding the patient’s background helps narrow down the diagnosis. Key aspects to assess include:Cough duration – to distinguish between acute and chronic forms
Smoking history – as chronic bronchitis is strongly associated with tobacco use
Recent infections – especially viral respiratory illnesses
Occupational exposure – to dust, fumes, or chemicals that may irritate the airways
Physical Examination:
A detailed chest examination may reveal classic respiratory signs such as:Wheezing – due to narrowed or obstructed airways
Prolonged expiratory phase – often seen in obstructive lung disease
Scattered rhonchi – coarse breath sounds caused by mucus in the airways
Laboratory tests
Laboratory investigations help differentiate between viral and bacterial causes, assess underlying conditions, and guide treatment decisions:
Complete Blood Count (CBC):
A routine blood test that can offer valuable clues:
An elevated white blood cell (WBC) count may indicate a bacterial infection.
Eosinophilia (increased eosinophils) can suggest an allergic or asthma-related component.
Sputum Culture and Gram Staining:
These tests are recommended when a bacterial infection is suspected:
Helps identify the specific pathogen and determine antibiotic sensitivity.
Particularly useful in chronic bronchitis patients with frequent exacerbations.
Viral PCR Tests:
Polymerase chain reaction (PCR) assays are used to detect viral pathogens with high accuracy:
Common targets include the influenza virus, RSV, rhinovirus, and coronavirus.
These tests are especially helpful during flu season or outbreaks.
Imaging
Imaging studies and lung function tests are crucial for ruling out serious conditions and confirming chronic bronchitis in appropriate cases:
Chest X-ray:
Often used to evaluate patients with persistent or severe symptoms:
Usually normal in acute bronchitis, helping to differentiate it from pneumonia.
Helps exclude other lung pathologies such as infiltrates, tumours, or signs of heart failure.
Pulmonary Function Tests (PFTs):
Essential for diagnosing and assessing chronic bronchitis and COPD:
Measures lung volumes and airflow limitations.
A reduced FEV1/FVC ratio is a hallmark of obstructive airway disease, supporting the diagnosis of chronic bronchitis.
Treatment of Bronchitis
Management of bronchitis depends on whether it is acute or chronic, ranging from supportive care and medications to advanced therapies like pulmonary rehab and surgery in severe cases.
Pharmacologic Therapy
The choice of medication in bronchitis depends on whether the condition is acute and self-limiting or chronic and progressive, often requiring long-term management.
For Acute Bronchitis:
Focuses on symptomatic relief, as most cases are viral and resolve on their own.
Supportive Care:
Adequate hydration, rest, and humidified air to ease symptoms.
Antipyretics:
Paracetamol (500–1000 mg every 6 hours) to reduce fever and discomfort.
Cough Suppressants:
Dextromethorphan (15–30 mg every 6 hours) for managing dry, irritating cough.
Expectorants:
Guaifenesin (200–400 mg every 4 hours) to loosen and clear mucus.
Antibiotics (Only if Bacterial Infection is Suspected): Not routinely recommended unless clinical signs point to bacterial involvement.
Amoxicillin-Clavulanate (875 mg/125 mg twice daily)
Doxycycline (100 mg twice daily for 5–7 days)
For Chronic Bronchitis: Treatment is aimed at improving airflow, reducing inflammation, and minimising exacerbations.
Bronchodilators:
Short-acting Beta-Agonists (SABAs): Albuterol (90 mcg, 2 puffs as needed)
Long-acting Beta-Agonists (LABAs): Salmeterol (50 mcg twice daily)
Inhaled Corticosteroids:
Combination therapy such as Budesonide/Formoterol (160/4.5 mcg twice daily) helps reduce airway inflammation.
Mucolytics:
Acetylcysteine (600 mg daily) to break down mucus and improve expectoration.
Supportive Therapy
Non-pharmacological interventions play a key role in managing chronic bronchitis, especially in improving quality of life and preventing disease progression:
Smoking Cessation:
The most crucial step in managing chronic bronchitis. Quitting smoking slows disease progression and reduces the frequency of exacerbations.
Pulmonary Rehabilitation:
A structured program that combines exercise training, education, and breathing strategies.
It helps enhance lung function, build stamina, and reduce hospital admissions.
Oxygen Therapy:
Recommended for patients with chronic bronchitis and hypoxemia (low blood oxygen levels).
Long-term use improves survival, especially in severe COPD cases.
Surgical Interventions
In advanced cases of chronic bronchitis, especially when associated with end-stage COPD, surgical options may be considered to improve breathing and quality of life:
Lung Volume Reduction Surgery (LVRS):
Involves removing damaged, non-functioning lung tissue to allow healthier lung areas to expand and work more efficiently.
Typically reserved for select patients with severe, localised emphysema.
Lung Transplantation:
Considered in end-stage, refractory cases where all other treatments have failed.
May significantly improve survival and daily functioning in eligible patients.
Statistical Data
Understanding the prevalence and risk factors of bronchitis highlights its public health significance and reinforces the importance of early intervention:
Global Prevalence:
Acute bronchitis is responsible for approximately 5% of all adult outpatient visits each year.
Chronic bronchitis affects nearly 9.3 million individuals in the United States alone, making it a major component of the chronic respiratory disease burden.
Smoking as a Risk Factor:
About 80% of chronic bronchitis cases are directly linked to smoking, underscoring the need for aggressive tobacco cessation programs.
Clinical Case
Patient Profile
- Age/Sex: 55-year-old male
- Medical History: 30-pack-year smoking history; chronic cough persisting for over 2 years
- Presenting Symptoms: Worsening productive cough, yellowish sputum, and intermittent wheezing
Diagnostic Workup
- Chest X-ray: Hyperinflated lungs; no signs of consolidation or infiltrates
- Pulmonary Function Tests (PFTs): FEV1/FVC ratio of 65%, consistent with obstructive airway disease (chronic bronchitis)
- Sputum Culture: Positive for Haemophilus influenzae, indicating bacterial involvement in acute exacerbation
Treatment and Outcome
Medications Prescribed:
- Salmeterol/Fluticasone inhaler for bronchodilation and inflammation control
- Azithromycin to address the acute infectious component
- Smoking cessation counselling as part of long-term disease management
Outcome: Marked improvement in symptoms with fewer exacerbations noted during follow-up visits
References
- Centers for Disease Control and Prevention (CDC). "Bronchitis Overview." Available at: cdc.gov
- World Health Organization (WHO). "Chronic Respiratory Diseases." Available at: who.int
- American Lung Association. "Bronchitis Facts and Figures." Available at: lung.org
- "Bronchitis Symptoms and Treatment." Available at: www.healthline.com
- Dr. Darshit Patel
- Chronic Diseases,Medicine and Diseases
- 16 August 2025
- 11:00








