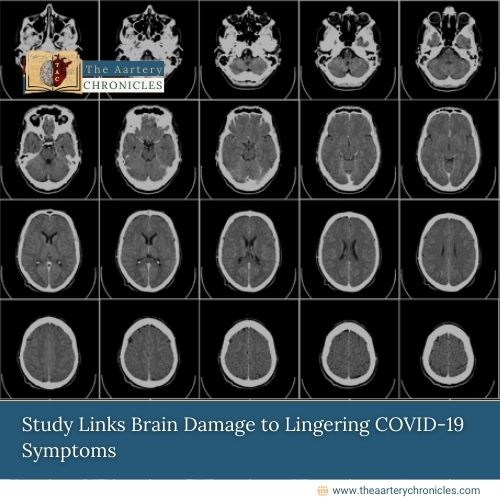
Study Links Brain Damage to Lingering COVID-19 Symptoms
Reading Time: 2 minutes The researchers found that various parts of the brainstem—the medulla oblongata, pons, and midbrain—showed signs of neuroinflammation
Study Links Brain Damage to Lingering COVID-19 Symptoms Read More »
Health News, People Forum