Benign Prostatic Hyperplasia (BPH)
Introduction
Benign prostatic hyperplasia (BPH), also known as an enlarged prostate, is a medical condition that affects men as they age. It involves non-cancerous (benign) enlargement of the prostate gland and is a common cause of lower urinary tract symptoms (LUTS) in older men. BPH is also known by the terms benign prostatic hypertrophy or benign prostatic obstruction.
In this article, we will understand the causes, symptoms, diagnosis, and treatment options that are crucial for managing this condition effectively.
The Prostate Gland: A Brief Overview
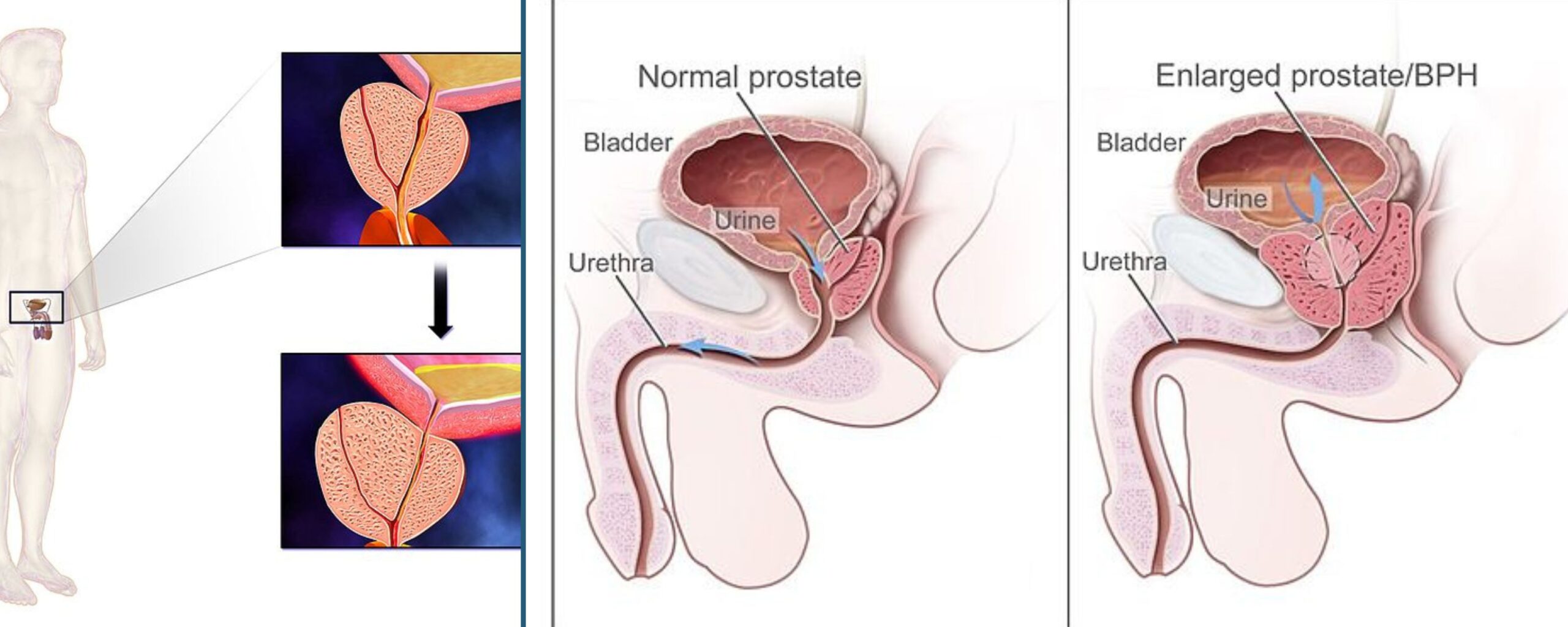
The prostate gland is a small, walnut-shaped organ that is a vital component of the male reproductive system. It is located below the urinary bladder and in front of the rectum in men. The prostate gland encircles a portion of the urethra at the junction (neck) of the urinary bladder. Both the urinary bladder and urethra are integral parts of the lower urinary tract. The urethra is a tube responsible for transporting urine and sperm out of the body. The primary role of the prostate is to produce prostate fluid, which contributes to semen. This fluid nourishes and transports sperm during ejaculation and is crucial for male fertility.
When the prostate gland enlarges, it can obstruct the flow of both urine and sperm through the urethra. While BPH itself is non-cancerous, its symptoms could potentially signify more serious conditions like prostate cancer.
What is Benign Prostatic Hyperplasia?
The prostate undergoes two main periods of growth as men age. The first phase of growth occurs during early puberty, when the prostate doubles in size. The second phase typically begins around age 25 and continues throughout most of a man’s life. Benign prostatic hyperplasia often develops during this later phase of growth.
As the prostate enlarges, the gland puts gradual pressure on and pinches the urethra. This compression can lead to thickening of the bladder wall. Over time, the bladder can weaken and fail to empty its contents completely. Urethral compression and bladder outflow obstruction result in lower urinary tract symptoms (LUTS) and urinary retention. Additionally, urinary stagnation in the bladder can also make men susceptible to urinary tract infections (UTIs) and bladder stones.
Symptoms of Benign Prostatic Hyperplasia
Symptoms related to an enlarged prostate that indicate benign prostatic hyperplasia often involve lower urinary tract symptoms. Some of these symptoms include:
- Frequent urination: An increased need to urinate, especially at night (nocturia).
- Urgency: A sudden and intense need to urinate.
- Difficulty starting urination: Trouble beginning to urinate despite the urge
- Weak urine stream: A weak or interrupted urine flow
- Urinary retention: Inability to empty the bladder completely after urinating
- Dribbling: Slow or delayed urine flow after finishing
- Urinary incontinence: Unintentional leakage of urine
- Discomfort after urination: Discomfort or pain following ejaculation or urination
Symptoms of benign prostatic hyperplasia usually stem from a blocked urethra and a bladder that becomes overworked from attempting to pass urine through this blockage.
Causes of Benign Prostatic Hyperplasia
The exact cause of benign prostatic hyperplasia (BPH) is unclear, but it primarily affects older men. BPH does not develop in men who had their testicles removed before puberty, leading the researchers to believe that factors related to aging and the testicles may contribute to the condition.
Throughout their lives, men continuously produce testosterone along with small quantities of estrogen. As they age, active testosterone levels drop, resulting in a higher proportion of estrogen. Studies suggest this higher estrogen proportion may increase substances that promote prostate cell growth, contributing to benign prostatic hyperplasia (BPH). Another theory involves dihydrotestosterone (DHT), a hormone crucial for prostate growth.
Another theory involves dihydrotestosterone (DHT), a hormone crucial for prostate growth. Despite lower testosterone levels, older men continue to produce high levels of DHT, which may stimulate continued prostate cell growth. Notably, men who do not produce DHT do not develop BPH.
Risk Factors for Benign Prostatic Hyperplasia
Risk factors for benign prostatic hyperplasia (BPH) include both non-modifiable and modifiable elements such as diabetes, diet, genetics, localized inflammation, obesity, and metabolic syndrome.
- Diabetes and antidiabetic medications: Diabetes and insulin use increase the risk of BPH, lower urinary tract symptoms (LUTS), and the need for prostatic surgery.
- Dietary Factors: Beta-carotene, carotenoids, and vitamin A may offer some protection against BPH, while excessive alcohol, caffeine, and high doses of vitamin C can increase risk and symptoms.
- Family History: Genetic predisposition may increase the risk of BPH.
- Localised Inflammation: BPH is often associated with localized inflammation, potentially due to factors like increased detrusor voiding pressure, obesity, chronic prostatitis, prostatic duct compression, and autoimmune disorders. NSAIDs can modestly improve BPH symptoms.
- Obesity: Observational studies link obesity to an increased risk of BPH, likely due to systemic inflammation and higher estrogen levels.
- Metabolic Syndrome: Conditions like hypertension, insulin resistance, and dyslipidemia are associated with larger prostate volumes. Elevated HbA1c levels also increase LUTS risk, but further studies are needed to clarify the relationship between diabetes and LUTS.
How is benign prostatic hyperplasia diagnosed?
Diagnosing Benign Prostatic Hyperplasia (BPH) involves a combination of medical history, physical examination, and specific tests. Here’s a comprehensive overview of the diagnostic procedure:
Medical history and symptom assessment: The doctor will begin by taking a thorough medical history and asking about symptoms. Patients may be asked to fill out the American Urological Association (AUA) Symptom Score questionnaire to quantify the severity of their lower urinary tract symptoms (LUTS) using questions that may include “Over the past few months…”
- How often have you felt unable to completely empty your bladder after urinating?
- How frequently have you needed to urinate again within two hours of finishing?
- How often have you experienced stopping and starting multiple times while urinating?
- How frequently have you found it difficult to delay urination?
- How often have you had a weak urine stream?
- How often have you needed to push or strain to begin urinating?
- How many times do you get up to urinate between going to bed and getting up in the morning?
Physical Examination
Digital Rectal Exam (DRE): This exam involves a physician inserting a lubricated, gloved finger into the rectum to assess the size, shape, and texture of the prostate gland.
Medical Tests
A urologist employs various medical tests to diagnose lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH) and to guide treatment recommendations. These tests may include:
- Urinalysis
- Prostate-specific antigen (PSA) blood test
- Cystoscopy
- Urodynamic tests
- Transrectal ultrasound
- Biopsy
How is benign prostatic hyperplasia treated?
Treatment options for benign prostatic hyperplasia (BPH) may involve lifestyle adjustments, medications, minimally invasive procedures, or surgical interventions.
Lifestyle Changes and Home Remedies for BPH
Certain lifestyle changes and home remedies can help manage mild BPH symptoms, including:
Limit fluid intake: Limiting fluid intake, especially in the evening, can reduce nighttime urination.
Reduce caffeine and alcohol: Both caffeine and alcohol can irritate the bladder and worsen the symptoms.
Exercise regularly: Physical activity can help maintain a healthy weight and reduce symptoms.
Bladder training: Practicing techniques to hold urine longer and urinate less frequently can help manage mild symptoms of BPH.
Medications for BPH
Alpha-blockers: These medications work by relaxing the muscles of the prostate and bladder neck, thereby improving the flow of urine.
5-Alpha Reductase Inhibitors: These medications block the production of DHT, a hormone that stimulates prostate growth.
Combination Therapy: Sometimes a combination of both types of medications is more effective.
Minimally Invasive Procedures for BPH
Researchers have introduced several minimally invasive procedures aimed at alleviating the symptoms of benign prostatic hyperplasia when medications are not effective. These procedures include:
- Transurethral needle ablation
- Transurethral microwave thermotherapy
- High-intensity focused ultrasound
- Transurethral electrovaporization
- Water-induced thermotherapy
- Insertion of prostatic stents
These techniques offer alternatives to traditional surgical methods for managing symptoms associated with enlarged prostate glands.
Surgical Interventions for BPH
For long-term management of benign prostatic hyperplasia (BPH), a urologist may suggest surgical interventions to either remove enlarged prostate tissue or widen the urethra by making incisions in the prostate. Surgical procedures to remove enlarged prostate tissue include:
Transurethral resection of the prostate (TURP): This procedure involves a urologist inserting a resectoscope through the urethra to visualize and remove excess prostate tissue, thereby alleviating urinary obstruction caused by benign prostatic hyperplasia (BPH).
Transurethral incision of the prostate (TUIP): This is a procedure where a urologist creates small incisions in the prostate and at the bladder neck through the urethra. This technique aims to widen the urethra and enhance urine flow in individuals suffering from BPH.
Laser Surgery: This procedure employs laser energy to vaporize or enucleate excess prostate tissue.
Open prostatectomy: Open prostatectomy involves making an incision in the lower abdomen to access and remove all or a portion of the prostate.
Complications of Benign Prostatic Hyperplasia
While most men with benign prostatic hyperplasia (BPH) do not experience complications, serious issues such as kidney damage can arise in some cases. Other potential complications include acute or chronic urinary retention, blood in the urine, urinary tract infections (UTIs), bladder damage, and the formation of bladder stones.
Conclusion
Benign prostatic hyperplasia is a common condition as men age, causing urinary symptoms that can impact daily life. Proper diagnosis and treatment can help manage the symptoms effectively, allowing men to continue their daily activities comfortably. If you experience symptoms of BPH, consult your healthcare provider to discuss the best management plan for you.









