
Understanding Osteoarthritis: Causes, Symptoms, & Management
Overview
As per the World Health Organisation (WHO), in the year 2019, an estimated 528 million people across the globe were living with osteoarthritis, reflecting a 113% increase since 1990. This significant increase highlights the growing global burden of the condition, making it essential to recognize its profound impact on daily life. Approximately, 344 million people with osteoarthritis experience varying degrees of severity that could benefit from rehabilitation interventions.
This article offers an in-depth understanding of osteoarthritis, including its causes, symptoms, diagnosis, and various treatment options to manage the condition better and improve overall well-being.
What Is Osteoarthritis?
Also referred to as wear and tear disease, OA is the most prevalent form of arthritis (a condition causing inflammation of joints) and is often seen in older adults.
Typically, the ends of bones in your joints, are shielded by a durable and smooth cartilage coating. By encasing the bone ends, the cartilage minimizes friction between the two bones along with serving as a shock absorber.
In OA, the cartilage wears down, gradually deteriorating all the joint components. As a result, the bones grind against each other when the joint is in motion leading to a range of symptoms.
What leads to Osteoarthritis?
- Aging: The risk of developing OA rises with age, as joints are subjected to prolonged, low-level stress which can gradually lead to wear and tear.
- Joint Injury: A previous joint injury can make an individual more susceptible to OA by disrupting the normal structure and function of the joint.
- Obesity: Excess body weight puts significant strain on your joints, especially hips and knees, as these areas bear more pressure, increasing the likelihood of OA.
- Repeated Stress: Sports that involve high-impact movements or heavy stress on the joints (Soccer, basketball) can further elevate the risk.
- Gender: It is more frequently seen in women than in men.
- Family History: OA often runs in families, suggesting a genetic predisposition.
- Health Conditions: Certain genetic conditions that affect joint function (Ehlers-Danlos Syndrome, Joint Hypermobility Syndrome) can predispose an individual to OA.
- Other Inflammatory Arthritis: Pre-existing joint inflammatory conditions such as gout, rheumatoid arthritis, and psoriatic arthritis can lead to the development of OA.
Recognizing Symptoms Of Osteoarthritis
The onset of osteoarthritis is typically gradual, with symptoms often intensifying as the condition evolves. It often manifests as:
- Pain: Movement can trigger or aggravate pain in the affected joints.
- Joint Stiffness: It is most pronounced after awakening (often lasts for less than 30 minutes) or following periods of inactivity.
- Tenderness: The joint may feel sore to touch when slight pressure is applied.
- Swelling: Soft tissue inflammation around the joint may lead to visible swelling.
- Reduced range of motion: Due to pain and stiffness, there can be a restricted range of motion in the affected joint, hindering normal movement.
- Friction-like sensation: Using the joint may produce a noticeable grating or crackling sensation.
- Joint Instability: The joint may feel unsteady or less stable than it normally does.
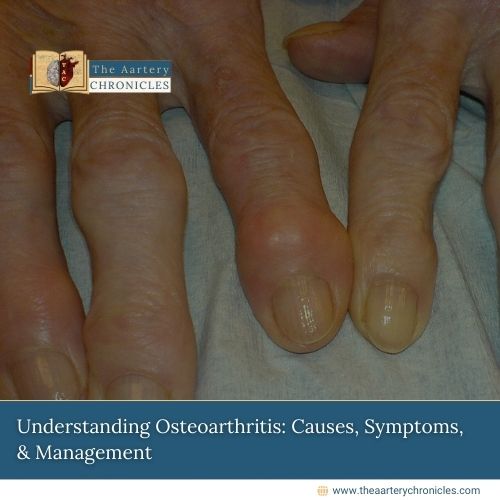
- Joint deformity: The joint may appear slightly distorted or have a knobby appearance.
Consequently, muscle strength often diminishes because of reduced movement, making it harder for individuals to perform physical activities. Thus, it becomes essential to take proactive steps in managing the condition and improving daily function.
Identifying Osteoarthritis: Diagnostic Approaches
Medical History
Your healthcare provider will inquire about the onset of your symptoms and if any specific factors make them better or worse. Additionally, they will also want to know if you have had any previous injuries or a medical condition that might contribute to your condition.
Physical Examination
The healthcare provider will assess the affected joint for pain, stiffness, and restricted range of motion. They will check for any crepitus (grinding noise) indicating friction between the bones. Also, any signs of muscle weakness or previous injury to the joint will be looked for.
Imaging Tests
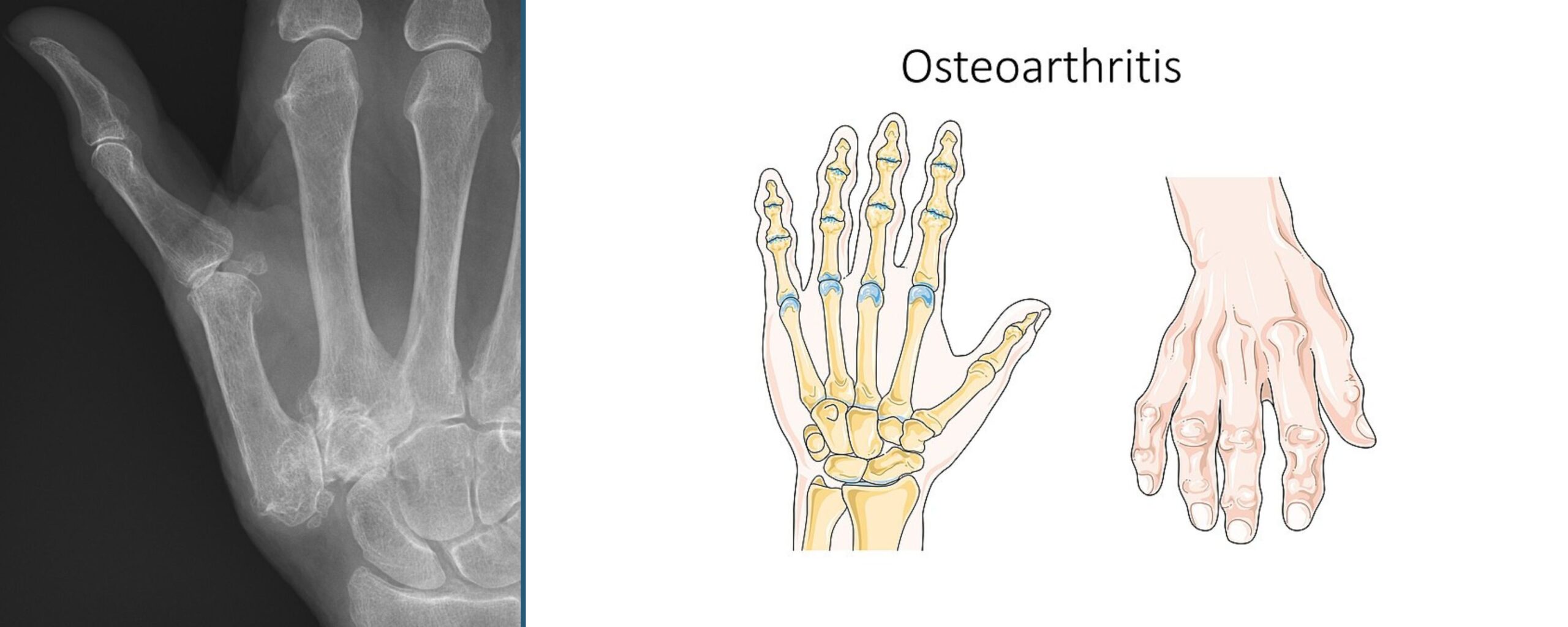
X-rays will be taken to evaluate the extent of joint damage. It can reveal
- Loss of Joint space (due to destruction of cartilage)
- Bone Erosion
- Formation of bone spurs (bony growths along the edges of the bone) around the joint.
However, in the early stages of the disease, X-rays often show no abnormalities as they lack the sensitivity to detect cartilage loss.
An MRI is not always required for diagnosis but it can help clarify complex cases by providing more detailed information.
Lab Tests
Blood tests cannot diagnose OA, but these are useful for excluding other potential causes that present with similar symptoms such as Rheumatoid Arthritis.
Managing Arthritis: A Treatment Overview
The management of osteoarthritis focuses on reducing pain, improving joint function, and preventing further damage to the joint. Here are a few key strategies:
Lifestyle Changes
- Regular exercise can help improve osteoarthritis by improving flexibility and reducing pain.
- Refrain from activities that provoke or intensify the pain.
- Low-impact activities such as stretching, cycling, and swimming should be considered. This will help strengthen the muscles around the joints, thus providing better stability and support.
- Losing weight (when needed) can also ease pressure on the weight-bearing joints such as the spine, knees, and hips.
Always consult a doctor or a physical therapist to ensure the chosen activities are safe and effective.
Supportive Devices
Splints and braces can provide support for weakened joints. Some are designed to restrict or prevent joint movement while others help redistribute pressure away from certain areas of the joint. However, they should only be used as recommended by your healthcare provider or therapist, as improper use can lead to further joint damage, stiffness, or increased pain.
Physical Therapy
Physical Therapy can be very helpful for patients in learning to use assistive devices (e.g., proper cane use) and in performing exercises. Exercise programs that combine aerobic and strength training have been shown to reduce pain and improve physical function and should be encouraged.
Pharmacotherapy
Although physical therapy plays a crucial role in managing the condition, pharmacological treatments can offer added benefits. Some of the medications commonly used in OA include:
- Acetaminophen: While treatment with Acetaminophen is considered modest and not clinically impactful, it can help alleviate symptoms in a minority of patients.
- NSAIDS: Drugs such as Ibuprofen and naproxen can provide substantial pain relief and should be used on an as-needed basis at first. However, they carry risks of stomach upset, gastric ulcers, gastric bleeding, and even kidney damage and are generally not suitable for long-term use. Topical NSAIDs (creams, gels) when applied directly to the affected joint, offer pain relief with a fewer side effect.
- Corticosteroid Injections: Since soft tissue inflammation is the main contributor to pain, injecting steroids directly into the affected joint can be highly effective in providing relief for a few months. These should be used with caution, as excessive use can lead to more harm than benefit.
Surgical Options
Most patients can achieve good outcomes and manage their condition effectively with conservative approaches, without the need for surgical intervention. But, in severe cases of OA, surgery may be considered to repair or replace the damaged joints. Surgical options include:
- Arthroscopic Surgery: In this procedure, the torn or damaged cartilage is removed.
- Osteotomy: This involves realigning the bones to reduce stress on the affected joint.
- Arthrodesis: It refers to the fusion of bones, often performed in the spine to provide stability.
- Joint Replacement Surgery: This involves replacing a damaged joint with a prosthesis, either partially or totally, to improve function. (E.g. Hip replacement, knee replacement, shoulder replacement surgeries).
Conclusion
The increasing prevalence of osteoarthritis poses a significant public health challenge. While no definitive cure exists, advances in treatment options that could halt the disease progression, offer renewed hope for those affected. Ultimately, a patient-centered approach, combining education, early diagnosis, and timely interventions is the key to mitigating the impact of osteoarthritis and improving long-term outcomes.
- Osteoarthritis - NHS
- What Causes Osteoarthritis, Symptoms & More | NIAMS
- Osteoarthritis - OrthoInfo - AAOS
- Osteoarthritis: MedlinePlus Medical Encyclopedia
- Osteoarthritis
- Osteoarthritis - Symptoms & causes - Mayo Clinic
- Osteoarthritis: Symptoms, Causes & Treatment Options
- Osteoarthritis - Diagnosis & treatment - Mayo Clinic

Dr Varsha Attri
MBBS
I’m a dedicated MBBS doctor with a strong passion for medical research. After graduating from SGRD University Of Health Sciences and working as a medical officer, I realized my passion for medical writing. I thrive on continuous learning and seek to expand my knowledge and skills in the field of Medical Journalism. Outside of medicine, I enjoy reading books and connecting with nature which fuel my creativity and inspire my writing. I’m eager to contribute meaningful content that informs and educates others in healthcare.