Know All About Uterine Fibroids: A complete guide
Overview
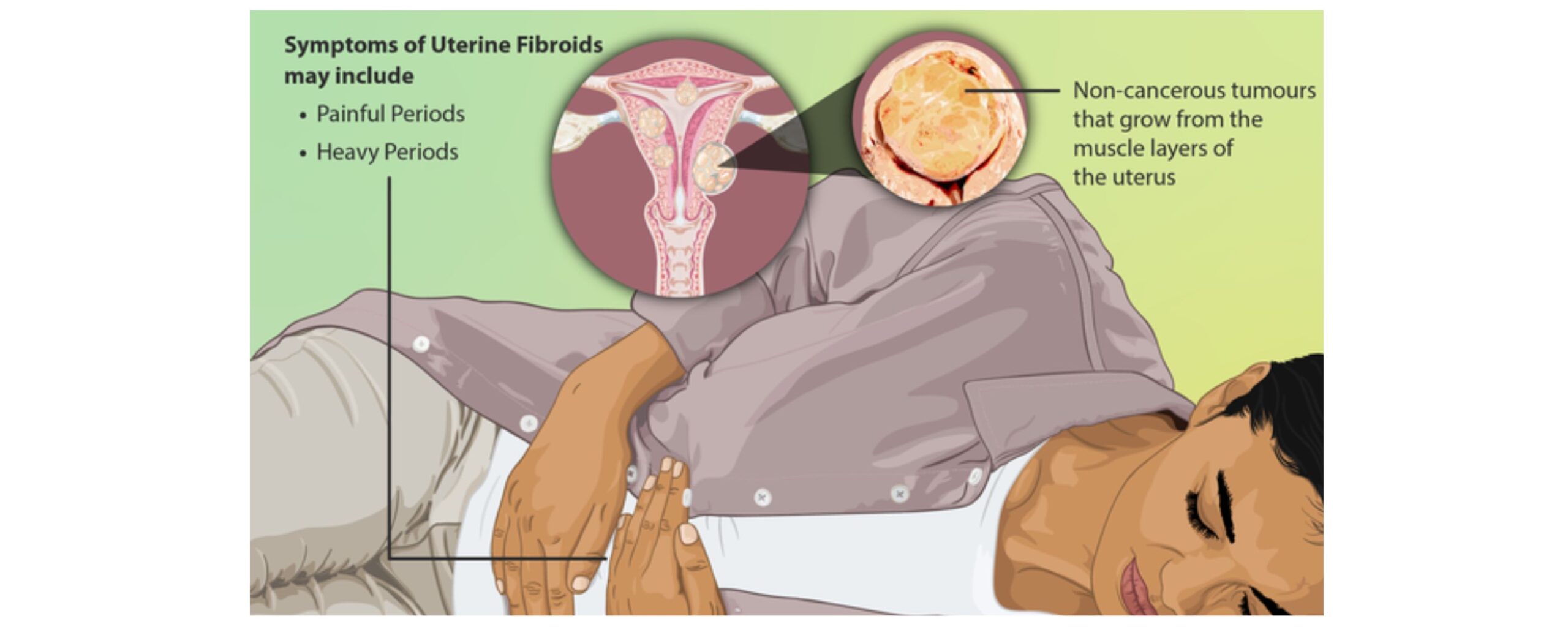
Also known as “leiomyomas,” fibroids are non-cancerous tumours that grow inside or around the uterus. These are one of the most prevalent benign growths among women of reproductive age affecting more than half of the women during their lifetime.
This article aims to provide valuable insights into uterine fibroids by exploring their potential causes, common symptoms, various diagnostic methods and the available treatment options to navigate the complexities of this condition.
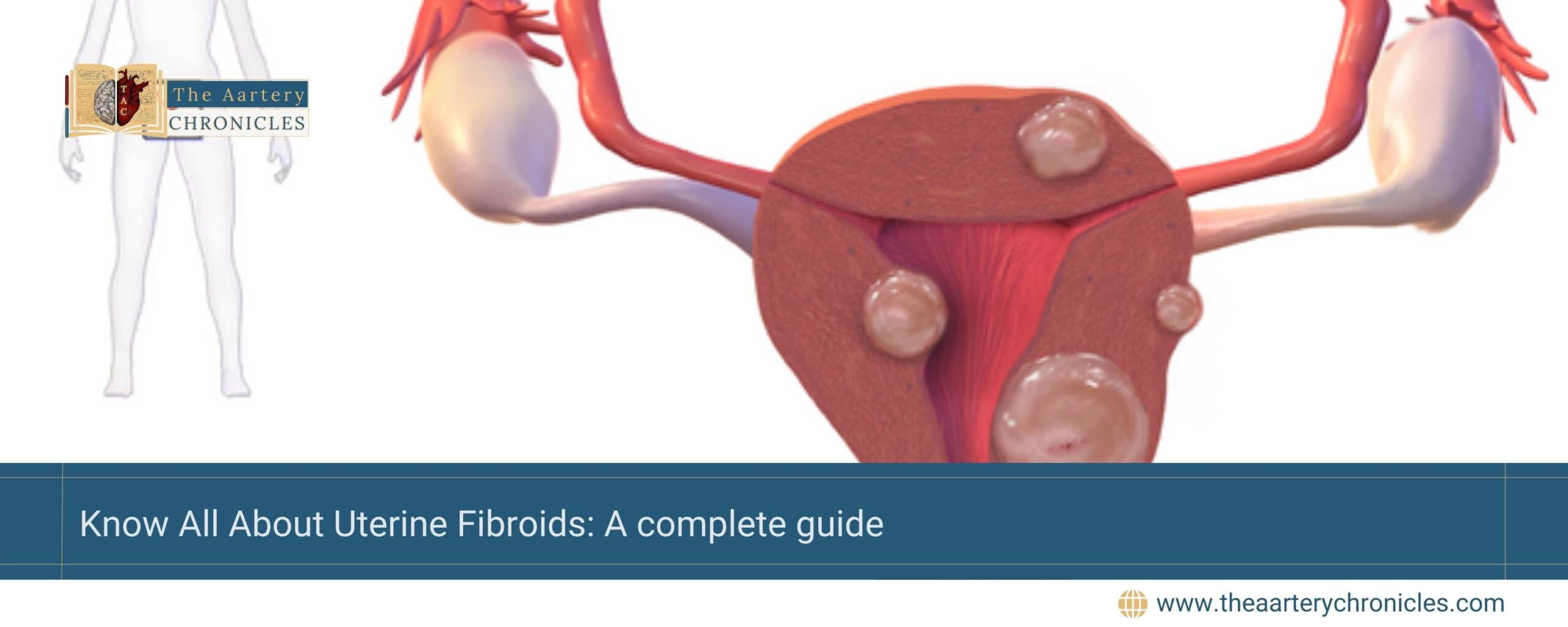
What are Fibroids ?
Fibroids are benign (non-cancerous) growths that originate in the muscle tissue of the uterus. They can vary widely in size, shape and number.
- Size: Some fibroids are small, only a few millimeters in diameter and may cause no symptoms while others can grow very large, thus, impacting the severity of the condition.
- Number: They can either appear as a solitary growth or occur in multiples, with numerous fibroids present within the uterus at once.
- Location: They may be located
- Inside the uterus
- On its surface
- Connected to it by a stalk-like structure (pedunculated fibroid)
Did you know that an estimated 20% to 50% of women of reproductive age have fibroids, and up to 77% may develop them at some point during their childbearing years? Interestingly, only about one-third of these fibroids are large enough to be identified during a physical exam, meaning many go undiagnosed.
Risk Factors for Developing Fibroids
Various risk factors contribute to the development of fibroids, ranging from genetic predisposition to lifestyle habits and hormonal influences. These include:
- Age: Fibroids are more prevalent as women get older, particularly in their 30s and 40s.
- Family History: If a woman has a family history of fibroids, her risk of developing them is higher. Specifically, if her mother or sister had fibroids, she is more likely to develop them herself.
- Ethnicity: African-American women have a higher likelihood of developing fibroids compared to white women.
- Obesity: Women with higher BMI (Body Mass Index) are at a greater risk for fibroids as carrying excess weight can lead to higher levels of oestrogen in the body.
- Dietary Patterns: A diet high in red meat such as beef or ham is associated with an increased risk for fibroids. Meanwhile, eating lots of green vegetables seems to offer some protection against developing them.
- Hormonal Influence: Fibroids are influenced by hormones such as estrogen and progesterone. They often stop growing or may shrink after menopause due to a decrease in estrogen levels. In contrast, hormonal medications can accelerate the growth of fibroids.
Recognising the Symptoms of Fibroids
Fibroids often go unnoticed, but when the symptoms do occur, they can range from mild discomfort to severe health issues. Some of the common symptoms include
- Excessive or heavy bleeding during your periods
- Periods lasting longer than usual or occurring more often
- Bleeding between menstrual cycles
- Increased menstrual cramping
- Anaemia due to blood loss
- Feeling of fullness in the lower abdomen
- Abdominal enlargement giving the impression of being pregnant
- Frequent urination
- Constipation
- Lower back pain
- Pain or discomfort during intercourse
In rare cases, a fibroid can cause sharp, severe pain if it grows too large for its blood supply and begins to degenerate. Fibroids can also cause complications during pregnancy and labour, with the risk of caesarean section being several times greater than usual. Thus, early recognition of these signs is essential for timely treatment and relief.
Diagnostic Methods for Identifying Fibroids
Most fibroids are diagnosed during a pelvic examination, where the doctor may feel for abnormal growths in the uterus.
- Doctors often describe the size of fibroids by comparing the uterus to how it would appear at certain weeks of pregnancy, such as saying it looks like a 12-week or 16-week pregnancy.
- Some fibroids are too small to be detected through a pelvic examination, which is why imaging tests are necessary to ensure they are not overlooked.
- Ultrasound is frequently used to diagnose fibroids, but MRI or CT scans may be recommended for more complex cases to provide detailed and clearer information.
Other techniques include
- Hysterosalpingography: In this procedure, a dye is injected into the uterus through the cervix which outlines the shape of the uterus and fallopian tubes. As the dye flows through these structures, a series of X-ray images are taken. This can help detect any blockages in the fallopian tubes or any structural abnormalities in the uterus, such as fibroids.
- Sonohysterography: It is also known as Saline Infusion Sonography. In this, a sterile saline solution is injected into the uterus through the cervix. This causes the uterine cavity to expand. Then ultrasound images are obtained which are more enhanced, allowing the doctor to better visualise the uterine lining and any potential abnormalities.
- Hysteroscopy: The inside of the uterine cavity is seen by inserting a thin, lighted device into the uterus. This helps to visualise any fibroids or polyps inside the uterus.
- Laparoscopy: This procedure is done under anaesthesia. Here, a small incision is made just below the belly button. A thin device (laparoscope) is inserted through the incision which aids the doctor in viewing pelvic organs in real-time and detect any abnormalities.
Treatment Options for Fibroids
When it comes to the treatment of uterine fibroids, the approach depends on various factors such as
- The size of fibroid
- Number
- Location of fibroid
- Symptoms experienced
- Patient’s age
- Reproductive plans
If fibroids are not causing any symptoms, treatment is typically not necessary. In these situations, a “watchful waiting” strategy may be recommended, where the condition is monitored over time to detect any changes or emerging symptoms. Intervention is considered only if the fibroids begin to cause any issues.
Medications
- Over-the-counter Drugs: In case of mild pain or discomfort, medications such as ibuprofen or acetaminophen can provide effective relief.
- Hormonal Therapy: It is often used to regulate menstrual cycles and manage the heavy bleeding and discomfort associated with fibroids. It can be administered in the form of
- Oral pills
- Injections
- Intra-uterine Devices (IUD)
- Iron Supplements: You may be required to take an iron supplement in case you have anaemia due to excessive blood loss.
- GnRHa (Gonadotropin Releasing Hormone Agonists): These include drugs like
- Leuprolide
- Goserelin
- Triptorelin.
They work by suppressing hormone production, which can lead to a reduction in the size of fibroids. With their use, women do not get periods, and anaemia often improves. However, side effects can occur, making long-term use (beyond six months) unsuitable, such as
- Hot flashes
- Vaginal dryness
- Bone loss
Taking low-dose oestrogen or progestin along with GNRHa, known as “addback Therapy” can help counteract these side effects and allow their use for up to 12 months.
- Tranexamic Acid: Another effective option for women experiencing heavy menstrual periods is Tranexamic Acid. It helps blood to clot and reduce excessive bleeding.
These treatments should be prescribed and monitored by a healthcare professional to ensure they are appropriate for your condition and to manage any potential side effects. Always seek medical advice before starting any medication for fibroids.
Surgical Treatment Options
Surgical options for fibroids are aimed at eliminating fibroids to alleviate symptoms like heavy bleeding, pain, and pressure on surrounding organs. These procedures improve the patient’s quality of life and include options like myomectomy or hysterectomy, depending on the individual’s needs and preferences.
- Myomectomy: This procedure is adopted to remove fibroids from the uterus while preserving the uterus itself. It is often recommended for women who wish to retain their fertility or avoid a hysterectomy. It can be performed through open abdominal surgery (laparotomy), laparoscopically, or via hysteroscopy.
- Hysterectomy: It is a surgical procedure in which the uterus is removed. It is considered a definitive solution for fibroids, effectively preventing their recurrence. This procedure is generally recommended for women who do not wish to have children in the future or when all other options have failed.
Minimally- Invasive Procedures
- Uterine Artery Embolization (UAE): In this procedure, tiny particles are injected into the blood vessels supplying blood to the fibroids, thus, blocking their blood flow and causing them to shrink.
- Radiofrequency Ablation (RFA): In RFA, a needle-like probe is inserted into the fibroid, using radiofrequency energy to heat and destroy the fibroid tissue. This leads to shrinkage of the fibroid and helps alleviate symptoms like heavy bleeding and pelvic pain. It is usually performed as an outpatient procedure. However, it is not recommended for women who want to preserve their fertility.
- MRI-guided Ultrasound Surgery: It is a relatively newer approach which uses MRI guidance to direct ultrasound waves precisely onto the uterus, targeting the fibroids without the need for any skin incisions. It reduces the size of the fibroids but it may not be as effective for very large ones.
Conclusion
Fibroids are a prevalent yet often manageable condition that can affect women’s reproductive health. Advances in diagnostic methods and treatment options offer hope for effective management tailored to individual needs. With proper diagnosis, treatment and appropriate care, most women can effectively manage their fibroids and maintain a good quality of life.

Dr Varsha Attri
MBBS
I’m a dedicated MBBS doctor with a strong passion for medical research. After graduating from SGRD University Of Health Sciences and working as a medical officer, I realized my passion for medical writing. I thrive on continuous learning and seek to expand my knowledge and skills in the field of Medical Journalism. Outside of medicine, I enjoy reading books and connecting with nature which fuel my creativity and inspire my writing. I’m eager to contribute meaningful content that informs and educates others in healthcare.








