Endometriosis Insights: Everything you need to know
Overview
Endometriosis is both a reproductive and systemic condition, often associated with severe pelvic pain, affecting an estimated 10% of women of reproductive age worldwide, which amounts to around 190 million women. [1, 2] Despite its prevalence, it is a commonly undiagnosed or misdiagnosed condition, primarily due to its highly variable symptoms, which are often associated with other disorders. [1] Endometriosis is primarily caused by the growth of endometrium-like tissue outside the uterine cavity. [3] It typically takes an individual around four to eleven years from the onset of symptoms to obtain a diagnosis and initiate treatment. [1]
This article aims to provide an in-depth analysis of endometriosis, focusing on its symptoms, causes, diagnosis, and treatment options, in order to raise awareness about this often-misdiagnosed condition.
What is Endometriosis?
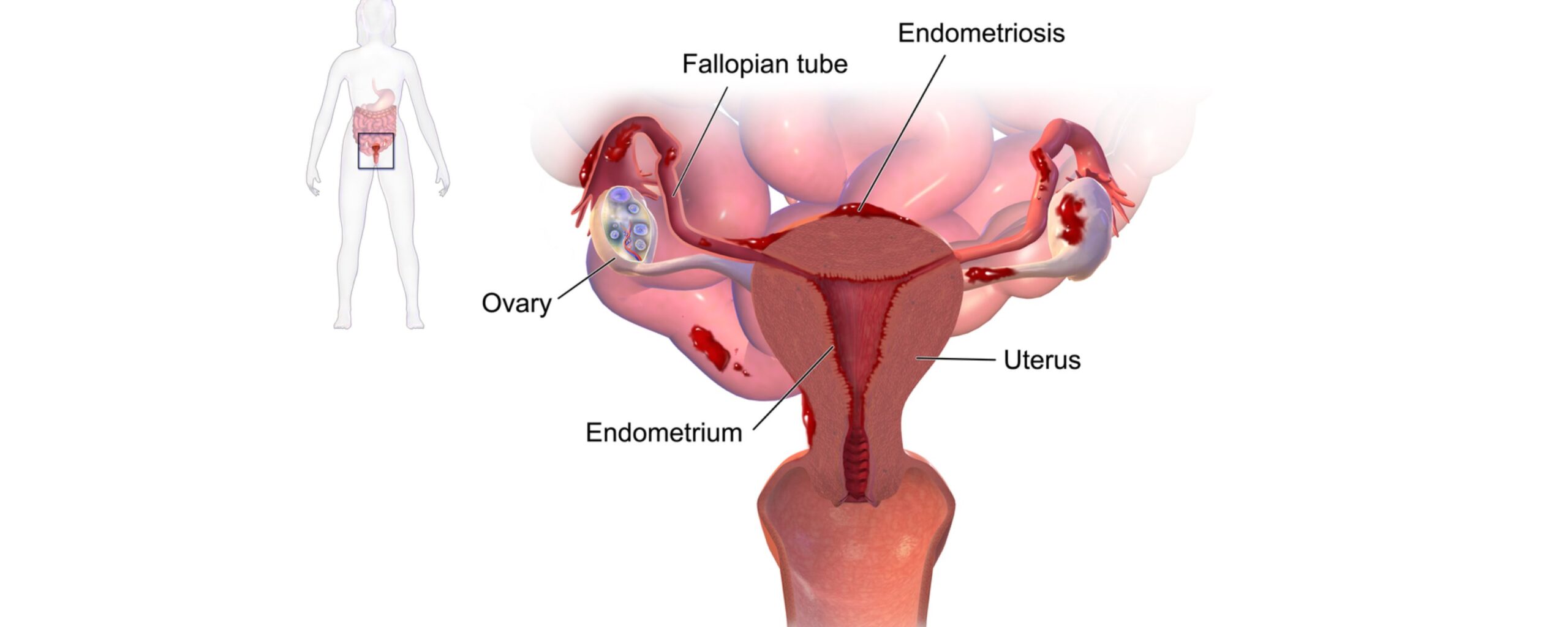
Endometriosis is an estrogen-dependent condition that occurs when tissue that resembles the inner lining of the uterus, known as endometrium, grows outside the uterus. The growth of this uterine tissue in the wrong places can cause painful symptoms that may impact not only the menstrual cycle but also interfere with daily life. [1, 4, 5]
The endometrium is the innermost lining of the uterus, also known as the womb, which plays a pivotal key role in the female reproductive system. During the menstrual cycle, hormones like estrogen stimulate the thickening of the endometrium in preparation for a fertilized egg. The endometrium breaks down if fertilization does not occur, and blood and endometrial tissue are expelled from the uterus through the vagina during menstruation. [1]
Endometriosis is also known by the condition “estrogen-dependent condition” because the endometrial growth outside the uterine cavity responds to menstrual cycle hormones, especially estrogen. Estrogen promotes growth and bleeding of endometrial tissue, including the extrauterine endometrial implants. This can lead to inflammation, the formation of scar tissue, and the development of adhesions that may cause pelvic tissues and organs to stick together [1, 3]
These extra-uterine implants and the resulting inflammation can cause pain, which may worsen before and during menstruation, as well as lead to heavy periods. The inflammation can also harm eggs and sperm, while the implants may block the movement of the egg through the fallopian tube and uterus, contributing to infertility and other complications. [1]
Endometriosis commonly occurs on or near reproductive organs in the pelvis or abdomen, including:
- Fallopian Tubes
- Ligament surrounding the uterus (uterosacral ligaments)
- Pelvic cavity lining
- Ovaries
- Outer surface of uterus
In rarer cases, endometrial tissue can also grow on and around the urinary bladder, cervix, intestines, rectum, stomach (abdomen), and even the vagina or vulva. [3]
What are the symptoms of endometriosis?
While symptoms of endometriosis can vary widely among individuals, pain and infertility are the two most common signs. Typical manifestations of endometrial symptoms include:
- Chronic pelvic pain
- Painful periods, also known as dysmenorrhea
- Pain may start before the period and continue during the entirety of the cycle, often worsening over time
- Heavy or irregular menstrual bleeding
- Pain during or after sexual intercourse (dyspareunia)
- Painful urination
- Pain while pooping
- Spotting or bleeding between periods
- Difficulty getting pregnant or infertility [1, 4]
Mood disorders, particularly anxiety and depression, are also linked to endometriosis. Some other symptoms of endometriosis include fatigue, low BMI (being underweight), and hypersensitivity to pain. [1]
Every individual’s experience with endometriosis is unique. Women with the condition may experience some, all, or none of these symptoms.
Risk Factors for Endometriosis
Certain factors that elevate an individual’s risk of developing endometriosis include:
- Family history of endometriosis (particularly first-degree relatives)
- Never having given birth
- Early onset of menstruation (before age 11)
- Short menstrual cycles (27 days or fewer)
- Heavy menstrual periods lasting longer than seven days
- Late onset of menopause [1, 4]
How is endometriosis diagnosed?
Diagnosing endometriosis can be difficult, as its symptoms often resemble those of other conditions. Common diagnostic steps include medical history examination by a physician, pelvic examination, and running imaging tests.
Medical History
Diagnosis of endometriosis typically begins with a review of the patient’s medical history. The doctor asks about symptoms, potential risk factors, and any difficulties the patient might be facing with conception. Questions about menstrual cycles are common, including whether the patient experiences painful periods, the time between cycles, the length of periods, and whether pelvic pain worsens during menstruation.
Physical Examination
The next part of the diagnostic process involves a physical examination, including a pelvic exam. During the pelvic exam, the doctor checks for signs of endometriosis, such as tenderness, pain, or a detectable lump near the ovaries.
Imaging Tests
Imaging tests such as an ultrasound, transvaginal ultrasound, or magnetic resonance imaging (MRI) are often recommended by physicians to help identify endometrial implants on the bowel, bladder, or other tissues.
Laparoscopy
Doctors may provide a “clinical diagnosis” of endometriosis based on medical history, physical exam findings, and imaging results. This allows treatment, such as hormonal contraceptives or pain relief, to begin without delay.
For a definitive diagnosis, however, surgical procedures like laparoscopy may be required. This minimally invasive method involves the insertion of a laparoscope (a long, thin tube equipped with a light and camera) to examine the pelvis and locate extra-uterine endometrial tissue and implants.
Biopsy
After identifying any suspicious tissue in the pelvis, a biopsy is performed to remove a sample, which is then sent to a laboratory for analysis. A biopsy is an essential diagnostic tool for obtaining a definitive diagnosis of endometriosis.
Management and Treatment for Endometriosis
Currently there is no cure or a lasting treatment available for endometriosis, but physicians can assist the patients with some treatment options that can alleviate the symptoms of the disease, shrink the endometrial implants, and in some cases, address fertility issues.
1. Medications
Pain relief medications: Since pelvic pain is one of the most common symptoms of endometriosis, pain relief medications such as NSAIDs and acetaminophen are commonly used to alleviate the pain associated with the condition. [1, 3]
Hormonal Therapies: Hormonal therapies help manage endometriosis by relieving pain and altering the body’s hormonal levels. [3] Hormonal treatment includes pills, shots, and nasal sprays. Some of the most common hormonal therapy options include:
- Combined oral contraceptives: Combination therapy (estrogen-progestin) along with NSAIDs is employed as the first-line treatment to relieve pain caused by endometriosis. Combined oral contraceptives help regulate menstrual cycles and reduce pain. [1]
- Progestin Therapy: Progestins help reduce endometriosis symptoms by shrinking endometrial growths. They are prescribed in patients that cannot or do not want to use combined oral contraceptives.[1]
- Gonadotropin-releasing hormone (GnRH) agonists or antagonists: GnRH agonists and antagonists work by reducing estrogen levels in the body, which helps suppress endometrial growth and menstruation while also alleviating pain associated with endometriosis. [1, 4]
2. Surgical Treatment
- Laparoscopy: Laparoscopy is a minimally invasive surgical procedure recommended for individuals with advanced endometriosis, persistent pain unresponsive to other treatments, or those seeking to improve fertility. It enables the surgeon to remove or destroy endometrial implants, adhesions, and scar tissue. [3]
- Hysterectomy: In severe cases, a hysterectomy, which is the surgical procedure for the removal of the uterus, may be considered. This is typically an option for women who no longer wish to have children. A physician might also advise oophorectomy (removal of ovaries) with or without hysterectomy. [3]
Oophorectomy is accompanied by significant reduction of estrogen levels, which can slow or halt the growth of endometrial tissue. However, this procedure carries menopause-related risks and side effects, such as hot flashes, bone loss, heart disease, reduced libido, memory issues, and mood disorders like depression or anxiety. [3] For these reasons, the decision to undergo oophorectomy is made collaboratively between the patient and their physician, considering individual circumstances and the patient’s personal objectives.
Conclusion
Endometriosis is a systemic, inflammatory condition characterized by chronically severe pelvic pain, heavy period flow, irregular or abnormal menstrual cycles, pain during or after sex, and infertility. Although endometriosis has no cure, the condition may occasionally resolve without treatment. Patients can achieve symptom relief through various treatment options, but endometrial tissue can regrow, and symptoms may recur even after surgery. Therefore, regular follow-ups with a doctor are recommended to monitor for signs of tissue regrowth or recurrence.









