What You Need to Know About PTSD: Causes, Symptoms, and Effects
What is PTSD?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition where individuals persistently re-experience trauma through nightmares and intrusive thoughts. It often occurs after exposure to actual or threatened death, serious injury, or sexual violation [I].
What are the Symptoms of PTSD?
The symptoms of PTSD may include:
- Persistent avoidance of stimuli associated with the traumatic event, such as distressing memories, thoughts, or feelings.
- Negative alterations in mood and cognition, including an inability to remember aspects of the event and distorted beliefs about its causes.
- Behavioural changes, such as irritability, aggression, recklessness, or self-destructive actions.

What are the Risk Factors for PTSD?
- History of childhood trauma
- Severity and nature of trauma
- History of poor coping mechanisms for stressful events
- Family history of trauma
- Low heart rate variability
- Low cortisol and other physiological variables
- Low IQ
Prevalence of PTSD in Youth
Approximately two-thirds of youth are exposed to trauma during childhood, with many developing PTSD as a result. By age 18, roughly 8% of traumatized youth meet the criteria for a PTSD diagnosis, with the numbers rising to 40% in cases of sexual abuse and assault. [2]

Neurobiological Findings in PTSD
In PTSD patients, there is a noticeable decline in hippocampus volume, increased amygdala reactivity, and decreased amygdala-prefrontal coupling with age. Abnormalities in the frontolimbic system, which includes brain regions involved in processing emotions and regulating stress responses, may contribute to heightened threat reactivity and weakened emotion regulation, particularly in pediatric patients with PTSD. [3]
PTSD and Chronic Illness
PTSD predisposes patients to chronic illnesses by increasing the risk of developing various physical health problems:
- Lack of sleep
- Physical symptoms such as obesity
- Comorbid depression
- Headaches
- Pain
For patients presenting with these physical symptoms, it is crucial to screen for a history of traumatic events to ensure an accurate diagnosis. [4]
Importance of Maternal Care in PTSD Prevention
Recent experiments have shown that maternal care is crucial to an individual’s development.
- Rat pups that received more licking and grooming from their mothers exhibited:
- Robust glucocorticoid receptor expression
- Lower levels of aggression
- When exposed to trauma, these rat pups developed PTSD at a lower rate than those deprived of maternal care.
This underscores the significant impact of maternal nurturing on stress resilience and mental health. [5]

What is Delayed PTSD?
Delayed PTSD is a form of Post-Traumatic Stress Disorder where symptoms do not fully manifest until some time after the traumatic event.
- A systematic review found that approximately 25% of patients experience a delayed onset of symptoms.
- Initially, these individuals may exhibit sub-threshold symptoms.
- Over time, these symptoms gradually increase in severity.
Typically, the symptoms reach the diagnostic threshold around six months after the trauma.
A Daunting Flashback… (This is a Fictional Story)
It was midnight when Malti saw a small girl playing with her Barbie doll in a dark room. The moonlight filtered into the room. She saw a shadow moving closer to the girl, absorbed in her play.
Before Malti could fully comprehend what was happening, she saw a man removing his clothes. She heard the rustle of the frock over the girl’s head and the girl’s frightened sobs as he touched her. After a while, the man walked out of the room, leaving the little girl weeping in a pool of blood. Malti stood there helplessly, watching the girl in pain. Why was it so difficult for Malti to help the girl? Why was she unable to stop the man?
By now, beads of perspiration had formed on Malti’s forehead. She felt numb, unable to breathe, and her voice seemed to be swallowed by the pool of blood surrounding the girl. When she opened her eyes, she realized it was a flashback to the sexual abuse she had endured when she was five, playing with her Barbie doll one night in her bed.
Today, at 19 years old, Malti still carries the trauma from her childhood, which continues to haunt her in adulthood. This trauma had overshadowed her childhood and was now affecting her adult life. She had wanted to escape it long ago but was too naive to understand what had really happened. By the time she understood and was ready to confront it, her mother told her it was her fault and advised her to forget about the incident.
Exhausted from these recurring traumatic flashbacks, Malti decided to seek help. She visited a psychiatrist and learned that she was diagnosed with PTSD. Determined, she believed that each experience offered an opportunity to reinvent herself and chose to pursue treatment.
What Did We Learn from This Story?
We learn that trauma and its consequences should not define the narrative of our lives. It is important to seek help and explore the treatment options available to combat PTSD. With the right support and therapy, individuals can take control of their healing journey and work towards a healthier future
Treatment of PTSD
A combination of treatments can effectively improve PTSD symptoms. [7]
Key approaches include:
- Skill Development: Teaching skills to manage symptoms and cope with potential relapses.
- Cognitive Restructuring: Helping individuals rethink their perceptions of themselves, others, and the world.
- Co-occurring Issues: Addressing related problems such as anxiety, depression, and substance misuse.
Cognitive Therapy
Cognitive therapy helps individuals identify and challenge negative thought patterns, such as harmful beliefs about oneself or fears of recurring trauma.
- It is often used alongside exposure therapy.
- The primary goal is to reshape these detrimental thought processes.
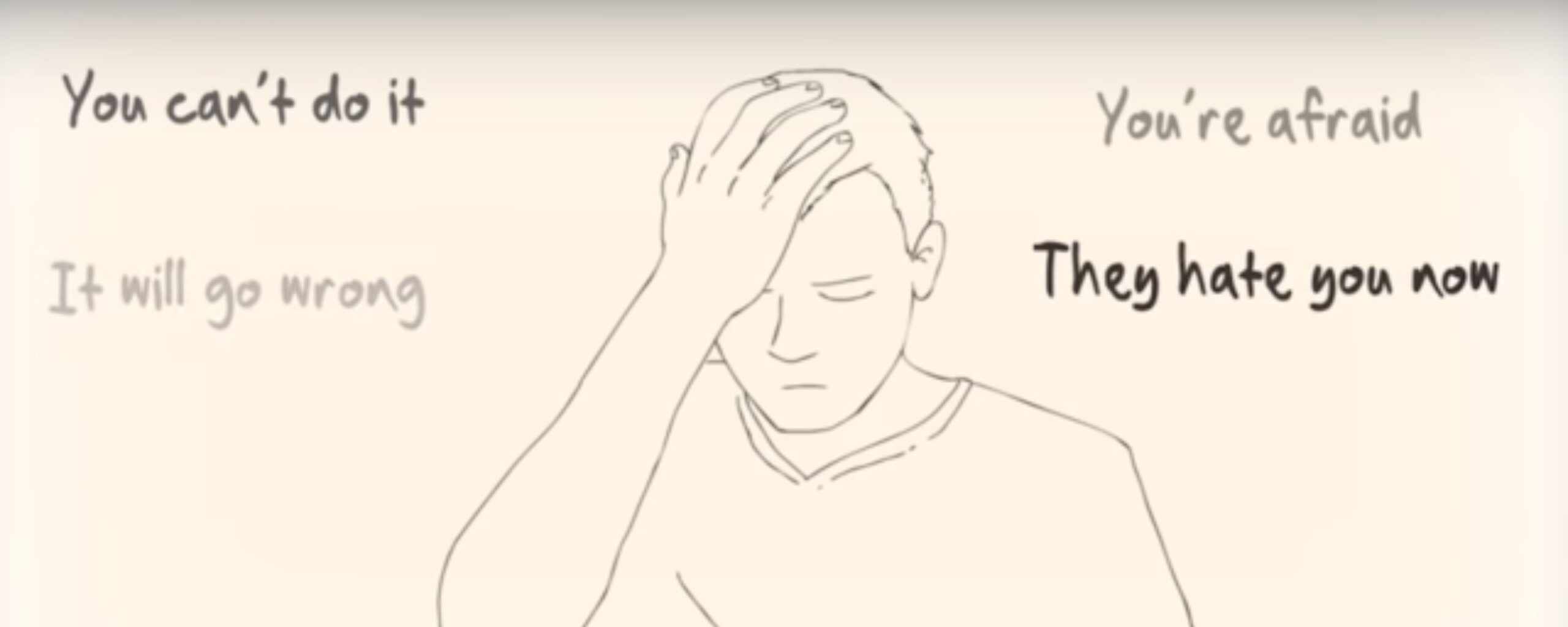
Exposure Therapy
Exposure therapy is a form of behavioural therapy that helps patients confront feared situations and traumatic memories in a controlled environment.
- This approach is particularly beneficial for managing symptoms such as flashbacks and nightmares.
- It enables individuals to cope more effectively with their trauma.
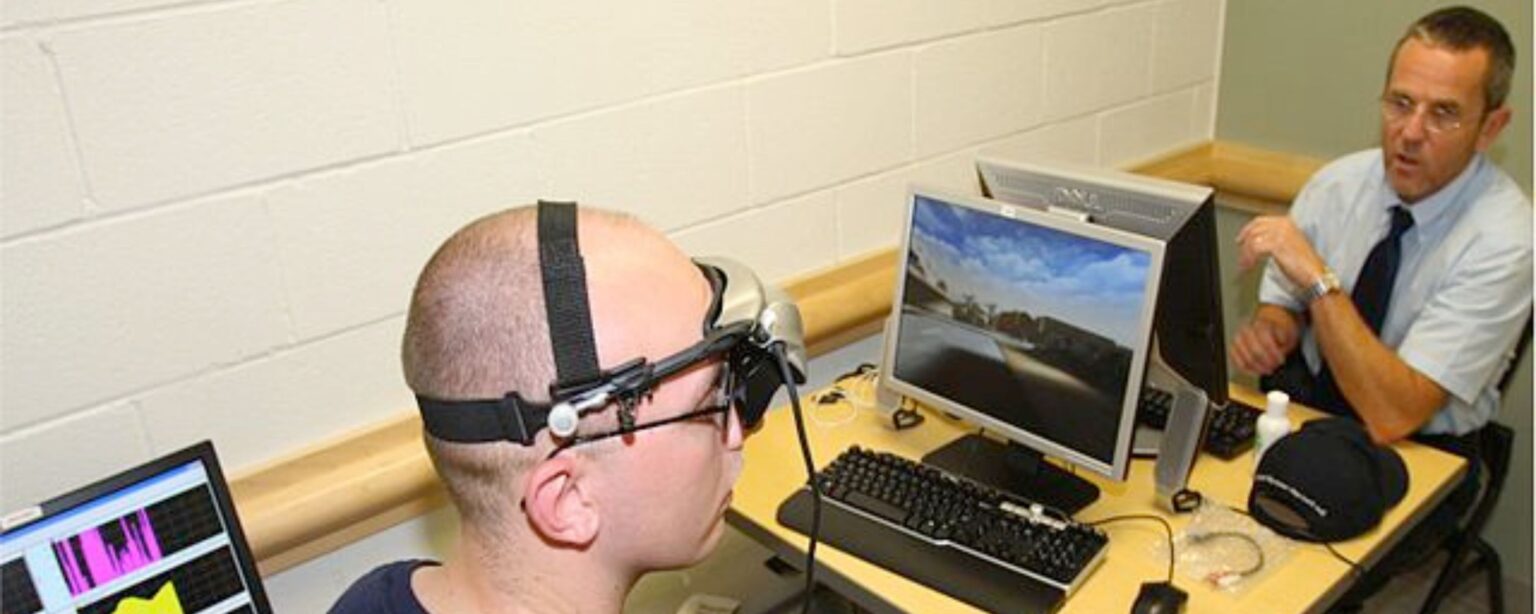
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR combines elements of exposure therapy with guided eye movements to facilitate the processing of traumatic memories. This technique helps individuals alter their emotional responses to these memories.
Medications
- Antidepressants: These medications, including selective serotonin reuptake inhibitors (SSRIs) like paroxetine and sertraline, can alleviate symptoms of depression and anxiety. They are approved by the Food and Drug Administration (FDA) for PTSD treatment.
- Anti-Anxiety Medications: These medications are used to relieve severe anxiety symptoms.
- Prazosin: Recent studies have shown that prazosin can be effective in treating PTSD, particularly symptoms like flashbacks and nightmares.
Conclusion
Post-Traumatic Stress Disorder (PTSD) is a complex condition that profoundly impacts individuals’ lives, manifesting through persistent trauma re-experiences, emotional dysregulation, and behavioral changes. Understanding the symptoms, risk factors, and neurobiological findings associated with PTSD is crucial for effective intervention and support.
Key treatment strategies, including cognitive therapy, exposure therapy, and medication, offer pathways to managing and mitigating the impact of PTSD. Additionally, factors such as maternal care and the recognition of delayed PTSD highlight the importance of early intervention and comprehensive care.
By acknowledging the complex nature of PTSD and exploring available treatment options, individuals and healthcare providers can work together to promote resilience, improve quality of life, and support healing.
With continued research and empathetic care, those affected by PTSD can find hope and the tools necessary for recovery.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, DC: American Psychiatric Publishing; 2013. p. 271-280
- opeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry. 2007;64(5):577-584.
Bremner JD. Traumatic stress: effects on the brain. Dialogues Clin Neurosci. 2006;8(4):445-461.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181836/
Schnurr PP, Green BL. Understanding relationships among trauma, post-traumatic stress disorder, and health outcomes. Adv Mind Body Med. 2004;20(1):18-29. Available from: https://pubmed.ncbi.nlm.nih.gov/15068106/
Weaver IC, Cervoni N, Champagne FA, D'Alessio AC, Sharma S, Seckl JR, et al. Epigenetic programming by maternal behavior. Nat Neurosci. 2004;7(8):847-854. doi:10.1038/nn1276. Available from: https://pubmed.ncbi.nlm.nih.gov/15220929/
Andrews B, Brewin CR, Philpott R, Stewart L. Delayed-onset posttraumatic stress disorder: a systematic review of the evidence. Am J Psychiatry. 2007;164(9):1319-1326. doi:10.1176/appi.ajp.2007.06091491. Available from: https://pubmed.ncbi.nlm.nih.gov/17728415/
American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. 2017. [Accessed July 2024]. Available from: https://www.apa.org/ptsd-guideline/ doi:10.1001/archpsyc.64.5.577. Available from: https://pubmed.ncbi.nlm.nih.gov/17485609/









