Vaginitis: What Women and Teenagers Should Know
Introduction
Let’s be honest — most of the time, you don’t think about your vagina. It does its job quietly, without demanding attention. But when something suddenly feels off — itching, burning, swelling, odd discharge, or pain — it quickly becomes impossible to ignore. Now your brain is on full alert, wondering What’s going on down there?
You’re not alone. These are all common signs of vaginitis, a condition many girls and women experience at some point. While it might feel uncomfortable to talk about, vaginitis is usually easy to treat — once you know what you’re dealing with.
In this guide, we’ll break down what vaginitis is, why it happens, and how to handle it — without panic, shame, or confusion.
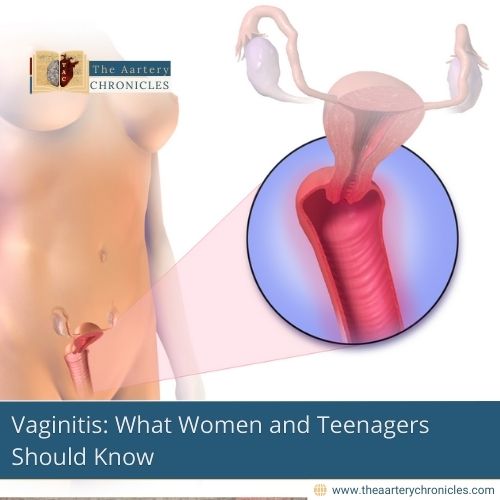
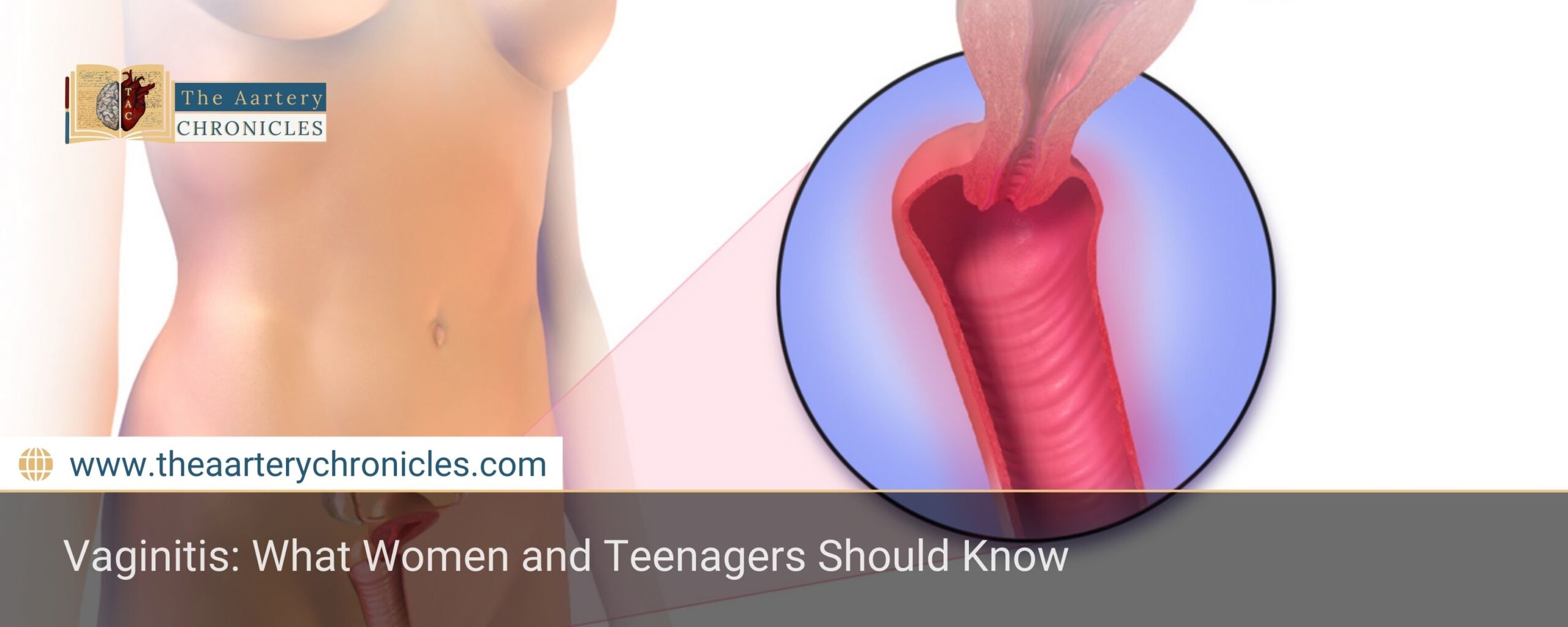
What Is Vaginitis?
Vaginitis is a condition marked by inflammation, infection, or irritation of the vagina. It can cause a multitude of uncomfortable symptoms like itching, a burning sensation, pain, discomfort, and abnormal discharge.
You might be surprised to learn that vaginitis isn’t caused by just one thing. In fact, it can happen for all sorts of reasons, from a disruption in the natural balance of bacteria in the vagina or even a reaction to things like scented soaps, creams, or laundry detergent. Sometimes, it’s linked to sexually transmitted infections (STIs) or vaginal dryness, especially in women with lower estrogen levels, like during menopause.
Vaginitis is incredibly common. Most women and teens will deal with it at least once — and often more than that — during their lifetime.
Types of Vaginitis
Understanding the different types can help you recognize what might be going on in your body:
1. Bacterial Vaginosis (BV)
- More common in women of reproductive age.
- Caused by an imbalance in natural vaginal bacteria.
- Symptoms: Thin, grayish-white discharge with a fishy odor.
2. Yeast Infections
- A yeast infection happens when there’s an overgrowth of Candida albicans, a type of fungus that normally lives in the vagina but can multiply too much under certain conditions.
- Symptoms: A dense, white discharge with a texture similar to cottage cheese, accompanied by itching, a burning sensation, and redness or irritation around the vaginal area.
3. Trichomoniasis
- Trichomoniasis is a type of sexually transmitted infection (STI) caused by a tiny parasite called Trichomonas vaginalis, which spreads through vaginal sex.
- Symptoms: Greenish-yellow, frothy, smelly discharge, vaginal itching, and burning.
4. Irritant or Allergic Vaginitis
- Allergic vaginitis occurs when the vagina reacts to certain products.
- This can be triggered by things like scented soaps, vaginal sprays, douches, fabric softeners, feminine hygiene products, wipes, or even lubricants.
- It can also be triggered by foreign objects like forgotten tampon, or toilet paper.
5. Atrophic Vaginitis
- Usually affects women after menopause when estrogen levels drop.
- It primarily affects women during their perimenopausal and postmenopausal stages of life.
- Symptoms: vaginal dryness, irritation, and painful intercourse.
Common Symptoms of Vaginitis to Watch For
Vaginitis doesn’t always look or feel the same. In fact, the symptoms can vary depending on the type, and sometimes, it doesn’t cause any symptoms at all. To make things trickier, it’s possible to have more than one type of vaginitis at the same time, like a yeast infection and bacterial vaginosis together.
Still, there are a few signs that show up across different types of vaginitis. If you notice any of these, your body might be telling you something’s off:
- Unusual vaginal discharge (different color, texture, or smell)
- Itching or irritation in and around the vagina
- A burning sensation, especially when you pee
- Redness or swelling around the vulva
- Discomfort or pain during sex or tampon insertion
- Light spotting or vaginal bleeding (not related to your period)
What Your Vaginal Discharge Is Telling You
It might feel awkward, but paying attention to your vaginal discharge can actually tell you a lot about your health. What you notice in your underwear or on toilet paper when you wipe can be one of the first signs that something’s off — especially when it comes to vaginitis.
Normal discharge is usually
- Clear, white, or off-white
- Has little to no odor
- Changes slightly throughout your menstrual cycle
Disruptions in your vaginal microbiome — the delicate balance of good and bad bacteria — can lead to changes in your vaginal discharge. Noticing these changes early can help you catch an infection before it worsens.
Here are some changes to look out for:
- Strong or unpleasant vaginal odor: Could be a sign of bacterial vaginosis or a sexually transmitted infection (STI)
- Clumpy, thick discharge (like cottage cheese): Common with a yeast infection
- Foamy or frothy discharge: Often a sign of trichomoniasis (a sexually transmitted infection)
- Green or yellow discharge: May point to an infection, especially if it’s also smelly or irritating.
Every vagina is unique, and your discharge might change slightly with hormones, birth control, or your cycle. But if something seems unusual for you — especially if it’s paired with itching, burning, or irritation — it’s a good idea to check in with a healthcare provider.
Risk Factors of Vaginitis
While vaginitis can happen to anyone, certain habits, health conditions, and lifestyle factors can make it more likely. Knowing the risk factors can help you take steps to prevent it or catch it early if it does happen.
You may be more likely to develop vaginitis if you:
- Recently used antibiotics or steroids
- Experience hormonal changes (puberty, pregnancy, menopause)
- Have unprotected sex or multiple partners
- Have a current or past STI
- Wear tight, damp, or sweaty clothing
- Use scented sprays, douches, or spermicides
- Have uncontrolled diabetes or a weakened immune system
How is vaginitis diagnosed?
To diagnose vaginitis, a healthcare provider will begin by taking a detailed medical and sexual history, including any past or current sexually transmitted infections (STIs). They will then perform a physical exam, which usually includes a pelvic exam to check for signs of irritation, discharge, or infection. During the pelvic exam, the provider may use a swab to collect a sample of vaginal discharge. The collected sample is then sent to a laboratory, where it’s analyzed to identify the cause of infection. In some cases, they may also test the pH level of your vaginal fluid, as this can help narrow down the diagnosis. For the most accurate results, you may be asked to avoid sexual activity or placing anything in your vagina (like tampons, creams, or douches) for at least 24 hours before your appointment.
How Is Vaginitis Treated?
Getting the right diagnosis is the first and most important step in treating vaginitis effectively. Since different types of vaginitis can share similar symptoms, it’s essential to pay attention to the specific details of your symptoms. Notice when they occur, the color, consistency, amount, and odor of your discharge — all of these can help your healthcare provider pinpoint the exact cause.
Once your provider knows what’s causing your vaginitis, they can recommend the best treatment plan for you:
Bacterial Vaginosis (BV)
If you have BV, your provider will likely prescribe antibiotics. These could be in the form of a vaginal gel or cream (like metronidazole or clindamycin) or oral antibiotics you take by mouth. These meds work by restoring the balance of good and bad bacteria in your vagina.
Yeast Infections
Over-the-counter (OTC) antifungal creams or vaginal suppositories are typically the first line of treatment for mild to moderate symptoms of yeast infections. However, it’s important to confirm that your symptoms are actually due to yeast before starting medication. Misdiagnosis can make things worse. If OTC treatments don’t work, your provider may recommend a stronger, oral antifungal like Diflucan.
Trichomoniasis
For trichomoniasis, a parasite-driven infection, your healthcare provider will prescribe oral antibiotics like metronidazole or tinidazole. Since trichomoniasis is contagious, partners from the past three months (or your most recent partner) will need to be treated as well to avoid reinfection.
Non-Infectious Vaginitis
If your vaginitis is caused by irritation (due to things like new soaps, scented products, or laundry detergents), the solution is simple: stop using the product causing the irritation. This might be all you need to do to clear things up.
Genitourinary Syndrome of Menopause (Atrophic Vaginitis)
If your symptoms are linked to low estrogen levels, especially during or after menopause, your provider may suggest prescription estrogen. Estrogen can be delivered in various forms, such as creams, tablets, or vaginal rings, all designed to improve the moisture and health of vaginal tissue.
Important: During treatment, it’s best to avoid sexual activity until your symptoms are completely gone or until your medication course is finished. This will help prevent further irritation or reinfection.
How to Prevent Vaginitis
- Skip the scented stuff. Avoid perfumed soaps, sprays, and bubble baths.
- Wear breathable underwear. Cotton is best.
- Change out of wet clothes. Don’t stay in swimsuits or sweaty gym clothes too long.
- Practice good hygiene. Gently wash the vaginal area with plain water or a mild, unscented soap. Avoid harsh cleansers or scented products, as they can disrupt your natural pH balance.
- Use condoms. They can help prevent sexually transmitted infections.
- Wipe front to back. This helps avoid spreading bacteria
Conclusion
Whether you’re a teenager experiencing these symptoms for the first time, or a woman managing changes in your body, vaginitis is nothing to fear. It’s common, manageable, and treatable. The most important thing is to listen to your body and speak up if something doesn’t feel right.
Remember: taking care of your vaginal health is just as important as caring for the rest of your body.