
Understanding Vaginismus: Causes, Symptoms, and Treatment
Introduction
Vaginismus is a condition characterized by involuntary contractions of the muscles surrounding the vagina, making penetration during intercourse, medical examinations, or even tampon use painful or impossible. This article explores the causes, symptoms, and available treatments for this complex but treatable condition.
What Is Vaginismus?
Vaginismus is a type of sexual pain and penetration disorder. Vaginismus is not simply a psychological aversion to sex, nor is it a deliberate response. Rather, it is an involuntary muscle contraction of the pelvic floor muscles that occurs when attempted penetration triggers a reflexive tightening response, making vaginal entry painful or impossible. The severity varies among individuals: for some, penetration may be uncomfortable, while for others, it is completely impossible.
There are two main types of vaginismus:
- Primary Vaginismus: This is when a person has never been able to achieve vaginal penetration without pain.
- Secondary Vaginismus: This occurs in individuals who previously had pain-free penetration but develop vaginismus later, often due to trauma, medical issues, or psychological stress.
Causes and Risk Factors of Vaginismus
Vaginismus may have both physical and psychological causes, and in many cases, the exact trigger is unclear. Some potential contributing factors include:
- Past sexual trauma or abuse
- Fear or anxiety related to sex
- Strict cultural or religious beliefs about sexuality
- Painful past experiences with penetration
- Childbirth injuries (vaginal tears)
- Medical conditions (e.g., infections, menopause, or pelvic surgery)
Psychological elements, such as fear of pain or performance anxiety, often perpetuate the physical reaction even if the original cause has resolved.
Symptoms of Vaginismus
The symptoms of vaginismus can vary in severity and presentation, but the most common include:
- Painful intercourse (dyspareunia): Often described as a burning, stinging, or tight sensation during vaginal penetration.
- Inability or difficulty inserting objects into the vagina: This may include fingers, tampons, or medical instruments.
- Involuntary muscle spasms in the vaginal area during penetration attempts.
- Pain during gynecological exams
- Long-term sexual pain with or without an identifiable physical cause
Triggering Activities
People with vaginismus may experience pain, discomfort, or anxiety during the following activities:
- Vaginal sex
- Oral sex (particularly if it involves touching or stimulation near the vaginal opening)
- Insertion of fingers
- Tampon use
- Use of vaginal dilators
- Pelvic or gynecological exams
The severity of the pain may range from mild discomfort to a sharp burning or tightening sensation. Importantly, vaginismus does not affect the ability to become sexually aroused or to reach orgasm through clitoral stimulation — the condition primarily affects penetrative activities.
Diagnosing Vaginismus
Diagnosing vaginismus typically begins with a detailed medical and sexual history, followed by a gentle and patient-centered pelvic exam, if tolerated. Because individuals with vaginismus often experience anxiety or physical resistance during exams, healthcare providers may use the Lamont-Pacik scale to assess the severity of the condition.
Lamont-Pacik Scale for Vaginismus Severity
This scale helps clinicians understand how the body responds during an attempted pelvic examination, ranging from mild discomfort to severe physical and emotional reactions:
- Lamont Grade 1: The individual is able to relax and allow a pelvic exam without significant discomfort.
- Lamont Grade 2: The individual is unable to relax enough for the exam to proceed.
- Lamont Grade 3: Involuntary responses occur, such as the buttocks lifting off the exam table and the toes curling upward in an attempt to avoid penetration.
- Lamont Grade 4: The individual tightly closes their thighs and lifts their buttocks to completely prevent the exam.
- Pacik Grade 5: There is a full-body response that includes severe emotional and physical distress, such as trembling, crying, hyperventilation, nausea, or vomiting, along with complete avoidance of the exam.
Understanding where a patient falls on this scale allows healthcare providers to tailor a treatment plan that addresses both the physical and emotional aspects of the condition.
Treatment Options for Vaginismus
Vaginismus is a highly treatable condition. Management focuses on reducing the involuntary muscle reflex that causes pelvic floor tightening while also addressing any underlying psychological or emotional factors, such as anxiety or fear related to penetration.
Healthcare providers may recommend a combination of the following evidence-based treatments:
Topical Therapy
Topical medications, such as lidocaine or specially compounded creams, may be applied to the vaginal area to reduce pain and discomfort during penetration attempts. These can help desensitize the area and improve comfort during early stages of treatment.
Pelvic Floor Physical Therapy
A specialized pelvic floor physical therapist works with the patient to help them identify, control, and relax the pelvic floor muscles through targeted exercises, manual techniques, and biofeedback.
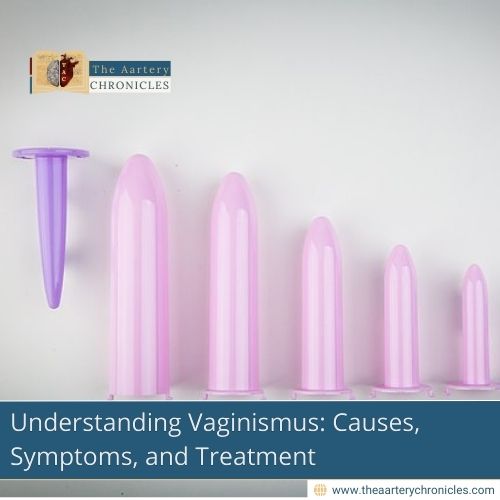
Vaginal Dilator Therapy
Vaginal dilators are tube-like devices of increasing sizes used to help gradually stretch the vaginal muscles. Patients begin with the smallest size and progress to larger ones over time. This therapy helps individuals become more comfortable with vaginal penetration. In some cases, a topical numbing cream is applied beforehand to ease the initial discomfort.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a well-established psychological treatment that helps individuals recognize and change negative thought patterns contributing to anxiety, fear, and avoidance behaviors. It is particularly effective for individuals with sexual trauma, post-traumatic stress disorder (PTSD), or negative associations with sexual activity, offering strategies to reframe distressing thoughts and support healthier emotional and behavioral responses.
Sex Therapy
Sex therapy, conducted by a licensed professional, supports individuals or couples in rebuilding trust, communication, and pleasure in their sexual relationships. Therapy may focus on exploring intimacy beyond penetration and reducing performance-related stress.
Conclusion
Vaginismus is a real and treatable condition. While it can be distressing, individuals experiencing it are not alone, and they are not “broken.” With the right care, understanding, and support, recovery is entirely possible.
If you suspect you may be experiencing vaginismus, consider speaking with a healthcare provider, therapist, or pelvic health specialist. Early diagnosis and a tailored treatment plan can lead to profound improvements in quality of life and sexual health.
- Vaginismus: MedlinePlus Medical Encyclopedia
- Case Series: Redefining Severe Grade 5 Vaginismus | Sexual Medicine | Oxford Academic
- Vaginismus: Dyspareunia, Causes, Symptoms, Treatment
- Examination of Treatment Duration, Treatment Success and Obstetric Results According to the Vaginismus Grades - PMC
- Physiotherapy for pelvic pain and female sexual dysfunction: an untapped resource - PMC
- Vaginismus Treatment: Clinical Trials Follow Up 241 Patients | Sexual Medicine | Oxford Academic
- Full article: Understanding vaginismus: a biopsychosocial perspective
- When Sex Is Painful | ACOG