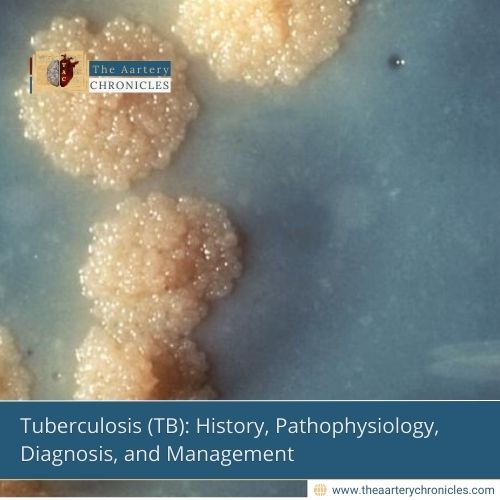

Tuberculosis (TB): History, Pathophysiology, Diagnosis, and Management
Excerpt
Tuberculosis (TB) is a chronic infectious disease caused by Mycobacterium tuberculosis, primarily affecting the lungs but capable of involving multiple organ systems. Despite advancements in treatment, TB remains a global health challenge, particularly in developing countries. This article explores the historical background, pathophysiology, clinical manifestations, diagnostic methods, and therapeutic approaches to TB.
ICD Codes and HCC Classification
- ICD-10 Codes:
- A15.0 (Tuberculosis of the lung, confirmed by sputum microscopy)
- A16.9 (Respiratory tuberculosis, unspecified)
- A19.9 (Miliary tuberculosis, unspecified)
- HCC Code: HCC 10 (Tuberculosis)
- Related Codes:
- Z11.1 (TB screening)
- Z22.0 (Carrier of tuberculosis)
History of Tuberculosis
- Evidence of TB dates back to 4000 BCE, with skeletal remains showing characteristic lesions.
- Ancient names: “Phthisis” (Hippocrates, 460 BCE), “Scrofula” (Middle Ages), “White Plague” (17th–19th century Europe).
- Robert Koch discovered Mycobacterium tuberculosis in 1882, revolutionizing TB diagnosis and treatment.
- The introduction of streptomycin (1944) and combination therapy significantly reduced TB mortality.
Definition
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis, transmitted via airborne droplets, leading to granulomatous inflammation in the lungs and other tissues.
Pathology
- Primary TB: Initial infection, often asymptomatic, leading to Ghon complex formation.
- Latent TB: Dormant infection with no symptoms but potential reactivation.
- Secondary (Reactivation) TB: Occurs in immunocompromised individuals, presenting with active disease.
- Miliary TB: Hematogenous spread of TB, leading to multiple organ involvement.
Types of Tuberculosis
- Pulmonary TB (Most common)
- Extrapulmonary TB:
- Lymph node TB (Scrofula)
- Skeletal TB (Pott’s disease)
- Meningeal TB (TB meningitis)
- Genitourinary TB
- Gastrointestinal TB
- Miliary TB (Disseminated TB)
- Multidrug-Resistant TB (MDR-TB) – Resistant to isoniazid and rifampicin
5. Extensively Drug-Resistant TB (XDR-TB) – Resistant to fluoroquinolones and second-line injectable drugs
Symptoms and Signs
- Pulmonary TB:
- Chronic cough (>3 weeks), hemoptysis, fever, night sweats, weight loss
- Pleuritic chest pain, dyspnea in advanced disease
- Extrapulmonary TB:
- Lymphadenopathy (Lymph node TB)
- Back pain, spinal deformities (Pott’s disease)
- Altered mental status, meningismus (TB meningitis)
Diagnosis
Laboratory Tests
- Urinalysis: Similar to other suppurative infections
- Blood tests: Leukocytosis with neutrophilia, elevated inflammatory markers (CRP, ESR)
- Biochemical tests: Assess metabolic and immune responses
Imaging
- Chest X-ray: Reveals a fluid-filled cavity with a surrounding capsule
- CT Scan: More sensitive for detecting abscess localisation and assessing adjacent structures
Differential Diagnosis
Lung abscess must be distinguished from:
- Lung Tumour: No fluid or gas in the lesion; lacks fever and malaise; may present as nodular growth
- Tuberculosis (TB): Typically affects the upper lobe of the right lung, presents with hemoptysis rather than purulent sputum, and has a diffuse “snow-like” lung appearance
Treatment
Standard First-Line Therapy (RIPE Regimen)
- Intensive Phase (2 months):
- Rifampicin (RIF) 10 mg/kg/day
- Isoniazid (INH) 5 mg/kg/day
- Pyrazinamide (PZA) 25 mg/kg/day
- Ethambutol (EMB) 15 mg/kg/day
- Continuation Phase (4 months):
- Rifampicin + Isoniazid
Drug-Resistant TB Treatment
- Multidrug-Resistant TB (MDR-TB): Resistant to RIF & INH, requiring second-line agents (e.g., Bedaquiline, Linezolid, Levofloxacin)
- Extensively Drug-Resistant TB (XDR-TB): MDR-TB with additional resistance to fluoroquinolones and injectables
Adjunctive Therapy
- Vitamin B6 (Pyridoxine) 25–50 mg/day (Prevents INH-induced neuropathy)
- Corticosteroids (For TB meningitis, pericarditis)
Surgical Interventions
- Lobectomy/Pneumonectomy: For non-resolving cavitary lesions, massive hemoptysis
- Pleural Drainage: In TB pleuritis with empyema
Statistical Data
- Global TB incidence: ~10.6 million cases/year (WHO 2022)
- TB-related deaths: ~1.6 million annually
- India, China, Indonesia: Highest burden countries
Clinical Case
Patient Profile:
- 45-year-old male, chronic smoker, presents with cough, weight loss, night sweats for 2 months
Findings:
- Chest X-ray: Cavitary lesions in upper lobes
- Sputum AFB positive
- GeneXpert: Rifampicin-sensitive TB
Treatment & Outcome:
- Started on 2HRZE/4HR regimen
- Significant improvement at 2-month follow-up with weight gain and symptom resolution
Mnemonics for Tuberculosis
- “RIPE” for TB Treatment:
- Rifampicin
- Isoniazid
- Pyrazinamide
- Ethambutol
- Symptoms – “Night Coughs With Fever”:
- Night sweats
- Cough (Chronic)
- Weight loss
- Fever
- Primary vs Secondary TB – “PRIMARY” vs “REACTIVATION”:
- Pleural effusion
- Recent exposure
- Infiltrates in lower lobes
- Mild symptoms
- Adenopathy
- Recoverable
- Young age
- Reactivation (Apical lesions)
- Elderly or Immunocompromised
- Advanced fibrosis
- Cavitation
- Treatment-resistant
- Indolent progression
- Older adults
- Night sweats
References

Author
Dr Darshit Jagdish Patel