
Medical Consent: Why Is It Necessary?
Introduction
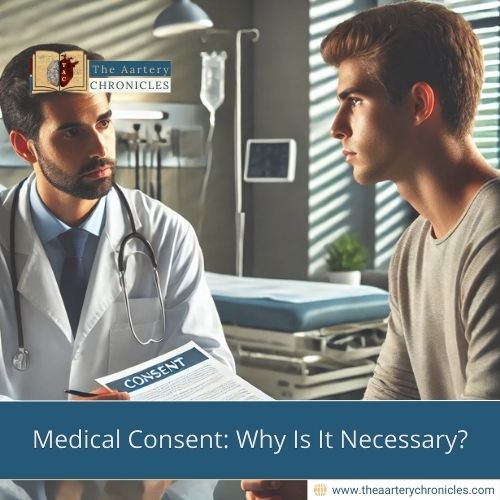
Imagine walking into a hospital, and without a word, the doctor immediately begins prepping you for surgery. You’d be confused, maybe even outraged. Now, flip the scenario—you’re the doctor. You know a procedure, like a blood transfusion, could save a patient’s life, but you can’t proceed without their consent. And sometimes, they refuse.
The Importance of Medical Consent
Consent is more than just a formality; it is a fundamental right. After all, why should you blindly trust a doctor with your life? What gives them the authority to make life-altering decisions on your behalf? Shouldn’t you have the opportunity to research and make an informed choice?
Your right to consent comes from the basic idea of your body, your choice. You should be able to decide what is good for you and what might harm you, and you should understand and accept the risks of any procedure. But what if the result of a procedure is the amputation of your leg? Why should you just accept that? You should always be able to ask questions, get clear answers, and understand your medical situation. This helps you make an informed decision and gives you peace of mind, not just for yourself, but also for your loved ones.
When Medical Consent Becomes a Barrier
While medical consent is essential, it can sometimes act as a barrier to care. For example, in an emergency where there is no time to obtain consent, a decision may need to be made quickly—such as performing an amputation to save a life. If I make that decision on your behalf, does it mean I am acting illegally, or am I simply doing what is best for my patient within the ethical framework that binds me as a healthcare provider?
Medical Consent in Paediatric Care
In a paediatric setting, where a guardian is a decision-maker, why should they be trusted with such important choices, especially when their decisions go against medical advice? Why can’t a doctor, who is trained and knowledgeable, decide what is best for the child? Why should a parent, who may be ill-informed, emotionally distressed, or influenced by religious beliefs, make decisions for a minor who has no choice but to accept their authority?
Autonomy vs. Medical Expertise
In a setting where you are making your own decisions, you have the power to say no—whether it’s because you don’t trust the doctor or because you read an article online or watched one of the TikTok doctors that contradicted your healthcare provider’s advice. Should your wishes be respected, or should the focus be on what will lead to your well-being?
Striking a Balance Between Rights and Care
Medical consent is a complex issue where patient autonomy and the need for timely care often collide. While respecting a patient’s decision is crucial, there are times when swift action is necessary to ensure the best possible outcome. Ultimately, the goal should be to find a balance that prioritizes the patient’s well-being, even if it means stepping in when a decision may not be in their best interest.

Author
Dr Toka Gamal