
Paws and Perils: The Hidden Hazards of Pet-Friendly Cafés
Balancing Companionship with Caution in Public Dining Spaces
Abstract:
Pet-friendly cafés have gained popularity across urban landscapes, offering a unique blend of social interaction and animal companionship. While they promote emotional well-being, they also present under-recognised public health risks, particularly in terms of zoonotic disease transmission, allergen exposure, and behavioural hazards. This article outlines the clinical implications, potential pathogens, allergic reactions, and regulatory concerns associated with pet cafés, aiming to provide medical insight for both healthcare professionals and the general public.
The global rise in pet ownership has led to a parallel boom in pet-friendly establishments, including cafés and restaurants that welcome animals. While these venues provide psychological benefits—such as reduced stress and enhanced mood—they also present a unique conjunction of veterinary and human medicine. Understanding the biological and behavioural risks is crucial for maintaining both public health and animal welfare.

1. Zoonotic Diseases: The Invisible Companions
Pets, particularly dogs and cats, can carry microorganisms transmissible to humans. In a shared food and social environment, the risk of zoonoses increases substantially.
Common Zoonotic Infections Reported:
There’s a new religion now: Productivity. Positivity. Personal Branding. We’re told to “manifest” our future, “biohack” our way to bliss. But no one tells us what to do with the unspoken grief, the inner child screaming behind our six-pack, or the silent shame of not being able to love yourself despite thousands of likes.
1. Campylobacter jejuni
Animal Reservoir:
Dogs and cats often carry Campylobacter jejuni in their gastrointestinal tracts.Human Risk:
Transmission occurs through contact with contaminated fur, saliva, or surfaces—especially if hands are not washed after handling pets.Clinical Manifestations:
Diarrhoea: Often watery or bloody, a hallmark of intestinal infection.
Abdominal cramps: Pain due to inflammation of the intestinal lining.
Other symptoms: Nausea, fever, and malaise may accompany the infection.
2. Salmonella spp.
Animal Reservoir:
Found in the intestines of dogs and reptiles (e.g., turtles, snakes, lizards), often without causing disease in the animals themselves.Human Risk:
Transmitted via the faecal-oral route, meaning ingestion of bacteria from contaminated hands, food, or surfaces exposed to pet faeces.Clinical Manifestations:
Fever: As part of the systemic inflammatory response.
Enteritis: Inflammation of the intestines leading to diarrhoea, abdominal pain, and vomiting.
Sepsis: A rare but serious complication if the infection spreads into the bloodstream.
3. Pasteurella multocida
Animal Reservoir:
A bacterium commonly found in the mouths of cats (and dogs), especially problematic when introduced into the body via bites or scratches.Human Risk:
Direct skin penetration through bites or scratches leads to rapid bacterial inoculation into tissues.Clinical Manifestations:
Cellulitis: A fast-spreading infection of the skin and underlying tissue, often within 24 hours of injury.
Soft tissue infection: Includes redness, pain, warmth, and swelling at the injury site.
Can occasionally lead to abscesses or systemic infection if untreated.
4. Toxoplasma gondii
Animal Reservoir:
Cats are the definitive hosts of this protozoan parasite, shedding infective oocysts in their faeces.Human Risk:
Infection occurs via ingestion of oocysts from contaminated soil, cat litter, undercooked meat, or unwashed vegetables.Clinical Manifestations:
CNS disease in immunocompromised individuals: Can cause encephalitis, seizures, or altered mental status.
Congenital toxoplasmosis: If a woman contracts the infection during pregnancy, the parasite may cross the placenta and harm the fetus, causing miscarriage, stillbirth, or neurological defects.
5. Dermatophytes (e.g., Microsporum canis)
Animal Reservoir:
Dogs and cats, particularly those with skin lesions, serve as reservoirs for dermatophyte fungi.Human Risk:
Transmitted through direct contact with infected animal fur, skin, or contaminated items like bedding or brushes.Clinical Manifestations:
Ringworm (Tinea corporis): A fungal skin infection, despite the name, not caused by worms.
Pruritic lesions: Itchy, red, ring-shaped patches with raised edges.
May involve the scalp, body, or nails depending on the site of exposure.
6. Bartonella henselae (Cause of Cat Scratch Disease)
Animal Reservoir:
Primarily domestic cats, especially kittens, which carry the bacteria in their saliva and claws.Human Risk:
Transmitted through scratches, bites, or contact with cat saliva on broken skin or mucous membranes.Clinical Manifestations:
Cat Scratch Disease (CSD): A bacterial infection that usually develops 3–10 days after the injury.
Lymphadenopathy: Swollen, tender lymph nodes near the site of the scratch or bite, often under the arm, neck, or groin.
Fever and malaise: Generalised symptoms that may mimic viral illness.
In immunocompromised individuals, it can cause more severe complications such as bacillary angiomatosis—a vascular skin lesion.
1. Campylobacter jejuni
Animal Reservoir:
Dogs and cats often carry Campylobacter jejuni in their gastrointestinal tracts.Human Risk:
Transmission occurs through contact with contaminated fur, saliva, or surfaces—especially if hands are not washed after handling pets.Clinical Manifestations:
Diarrhoea: Often watery or bloody, a hallmark of intestinal infection.
Abdominal cramps: Pain due to inflammation of the intestinal lining.
Other symptoms: Nausea, fever, and malaise may accompany the infection.
2. Salmonella spp.
Animal Reservoir:
Found in the intestines of dogs and reptiles (e.g., turtles, snakes, lizards), often without causing disease in the animals themselves.Human Risk:
Transmitted via the faecal-oral route, meaning ingestion of bacteria from contaminated hands, food, or surfaces exposed to pet faeces.Clinical Manifestations:
Fever: As part of the systemic inflammatory response.
Enteritis: Inflammation of the intestines leading to diarrhoea, abdominal pain, and vomiting.
Sepsis: A rare but serious complication if the infection spreads into the bloodstream.
3. Pasteurella multocida
Animal Reservoir:
A bacterium commonly found in the mouths of cats (and dogs), especially problematic when introduced into the body via bites or scratches.Human Risk:
Direct skin penetration through bites or scratches leads to rapid bacterial inoculation into tissues.Clinical Manifestations:
Cellulitis: A fast-spreading infection of the skin and underlying tissue, often within 24 hours of injury.
Soft tissue infection: Includes redness, pain, warmth, and swelling at the injury site.
Can occasionally lead to abscesses or systemic infection if untreated.
4. Toxoplasma gondii
Animal Reservoir:
Cats are the definitive hosts of this protozoan parasite, shedding infective oocysts in their faeces.Human Risk:
Infection occurs via ingestion of oocysts from contaminated soil, cat litter, undercooked meat, or unwashed vegetables.Clinical Manifestations:
CNS disease in immunocompromised individuals: Can cause encephalitis, seizures, or altered mental status.
Congenital toxoplasmosis: If a woman contracts the infection during pregnancy, the parasite may cross the placenta and harm the fetus, causing miscarriage, stillbirth, or neurological defects.
5. Dermatophytes (e.g., Microsporum canis)
Animal Reservoir:
Dogs and cats, particularly those with skin lesions, serve as reservoirs for dermatophyte fungi.Human Risk:
Transmitted through direct contact with infected animal fur, skin, or contaminated items like bedding or brushes.Clinical Manifestations:
Ringworm (Tinea corporis): A fungal skin infection, despite the name, not caused by worms.
Pruritic lesions: Itchy, red, ring-shaped patches with raised edges.
May involve the scalp, body, or nails depending on the site of exposure.
6. Bartonella henselae (Cause of Cat Scratch Disease)
Animal Reservoir:
Primarily domestic cats, especially kittens, which carry the bacteria in their saliva and claws.Human Risk:
Transmitted through scratches, bites, or contact with cat saliva on broken skin or mucous membranes.Clinical Manifestations:
Cat Scratch Disease (CSD): A bacterial infection that usually develops 3–10 days after the injury.
Lymphadenopathy: Swollen, tender lymph nodes near the site of the scratch or bite, often under the arm, neck, or groin.
Fever and malaise: Generalised symptoms that may mimic viral illness.
In immunocompromised individuals, it can cause more severe complications such as bacillary angiomatosis—a vascular skin lesion.
Reference:
- CDC Zoonotic Diseases: https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html
- Toxoplasmosis Info: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8897489/

2. Food Safety and Hygiene Concerns
Cross-contamination risks in pet cafés stem from:
- Pets on tables or chairs
- Shared utensils (e.g., water bowls for pets near human food)
- Lack of separation between food prep zones and pet activity areas
This creates a high-risk environment for foodborne illness transmission. Pets licking hands or food contact surfaces can introduce faecal bacteria to communal areas, especially when hand hygiene protocols are poorly enforced.
Evidence-based data:
A 2020 study in Food Protection Trends showed that cafés allowing animals on furniture had 25% higher surface contamination with Enterobacteriaceae compared to pet-free counterparts. ( https://www.foodprotection.org/publications/food-protection-trends/)

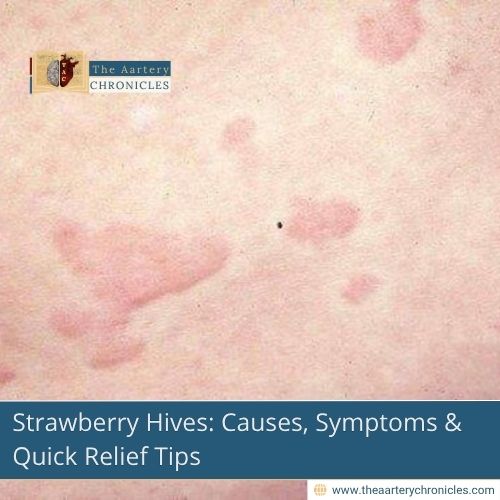
3. Allergy and Asthma Triggers
Animal dander is a potent allergen that persists in indoor environments long after the animal has left.
Potential outcomes in sensitive individuals:
- Asthma exacerbations
- Allergic rhinitis
- Atopic dermatitis flares
Clinical note:
Even minimal exposure to cat allergen (Fel d 1) can provoke symptoms in highly sensitive individuals. Asthma attacks may be triggered by airborne allergen particles, especially in enclosed or poorly ventilated spaces. (Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9186324/)

4. Behavioural and Physical Risks
While many pets are well-trained, animal behaviour is unpredictable, especially in crowded or overstimulating environments.
Common incidents reported:
- Dog bites or scratches due to territorial behaviour
- Pet-to-pet aggression, leading to owner injuries
- Food theft or food aggression, especially if pets are allowed to interact during mealtimes
Clinical Case Example
An urban café in Mumbai reported a canine-on-canine attack resulting in severe forearm laceration to the owner trying to intervene (unpublished case, 2023). This underscores the need for trained animal handlers or pet zoning inside such spaces.

5. Immunocompromised Individuals and Pregnancy
High-risk populations such as:
- Pregnant women
- Elderly
- Immunocompromised individuals (e.g., transplant patients, cancer patients)
…are especially vulnerable to zoonotic pathogens and allergen exposure. Even mild infections in immunocompetent individuals may cause severe systemic outcomes in these groups. (CDC Pet Safety Guidelines: https://www.cdc.gov/healthypets/publications/pet-safety-for-immunocompromised.html)

6. Regulatory Oversight: A Grey Zone
Most countries lack uniform public health regulations around pet-friendly cafés. While food safety norms exist, enforcement regarding live animal access in dining zones remains inconsistent.
Example:
- India’s FSSAI guidelines do not mention rules for animals in restaurants.
- The UK’s Food Standards Agency (FSA) allows pets but urges separate zones and strong hygiene policies.
There is a pressing need for clear SOPs addressing pet cafés, including:
- Mandatory vaccination and deworming records
- Designated pet areas with non-slip, easily cleanable surfaces
- Staff trained in both food hygiene and basic animal first-aid

Conclusion: Love Them, But Lead with Logic
Pet-friendly cafés offer a warm, inclusive experience for animal lovers. However, they are also complex microbiological ecosystems. For these environments to be truly safe and sustainable, public awareness, responsible ownership, and regulatory clarity are essential.
As medical professionals, we advocate for a model that respects both human health and animal joy, encouraging cafés to adopt evidence-based hygiene practices, clear pet-handling policies, and robust education around potential health risks.
- Dr. Darshit Patel
- Infectious Diseases,Medicine and Diseases,People Forum
- 16 August 2025
- 11:00