
Navigating the Frontiers of Antibiotic Resistance

Accidental Discovery of Penicillin
Sir Alexander Fleming accidentally discovered the substance with antibacterial properties in 1928. He noticed mould (Penicillium) inhibiting bacterial growth in a petri dish. The substance discovered by Fleming was later identified as penicillin by other researchers, most notably Howard Florey and his team, who conducted extensive research to produce and test penicillin's effectiveness.
Penicillin did play a crucial role in treating bacterial infections among soldiers during World War II, which helped save many lives. However, it's important to note that penicillin production on a larger scale and its widespread use occurred a few years after World War II.

Accidental Discovery of Penicillin
Sir Alexander Fleming accidentally discovered the substance with antibacterial properties in 1928. He noticed mould (Penicillium) inhibiting bacterial growth in a petri dish. The substance discovered by Fleming was later identified as penicillin by other researchers, most notably Howard Florey and his team, who conducted extensive research to produce and test penicillin's effectiveness.
Penicillin did play a crucial role in treating bacterial infections among soldiers during World War II, which helped save many lives. However, it's important to note that penicillin production on a larger scale and its widespread use occurred a few years after World War II.

Accidental Discovery of Penicillin
Sir Alexander Fleming accidentally discovered the substance with antibacterial properties in 1928. He noticed mould (Penicillium) inhibiting bacterial growth in a petri dish. The substance discovered by Fleming was later identified as penicillin by other researchers, most notably Howard Florey and his team, who conducted extensive research to produce and test penicillin's effectiveness.
Penicillin did play a crucial role in treating bacterial infections among soldiers during World War II, which helped save many lives. However, it's important to note that penicillin production on a larger scale and its widespread use occurred a few years after World War II.
Impact of Antibiotics on global health outcomes
With the discovery of antibiotics, diseases that were regarded as fatal or chronic became treatable. Antibiotics are used to stop or slow down the growth of bacteria. The discovery of antibiotics significantly lowered the death ratio. Over the time of 100 years, antibiotics have significantly changed the course of modern medicine. Antibiotics have played a significant role in increasing the average lifespan of humans by 23 years along with advances in healthcare, sanitation, nutrition, and various medical interventions.
Antibiotics have played a major role in the advancement of medicine and surgery. Antibiotics have been successful in treating and preventing infections in patients suffering from various ailments or issues such as diabetes, renal diseases, and arthritis. Antibiotics have also been prescribed to patients receiving chemotherapy, or patients who have undergone surgeries such as joint replacements, organ transplants, or cardiovascular surgeries. In countries that have relatively low living standards, and sanitation is poor, antibiotics help reduce morbidity and mortality that can be caused due to foodborne or other infections associated with poverty.
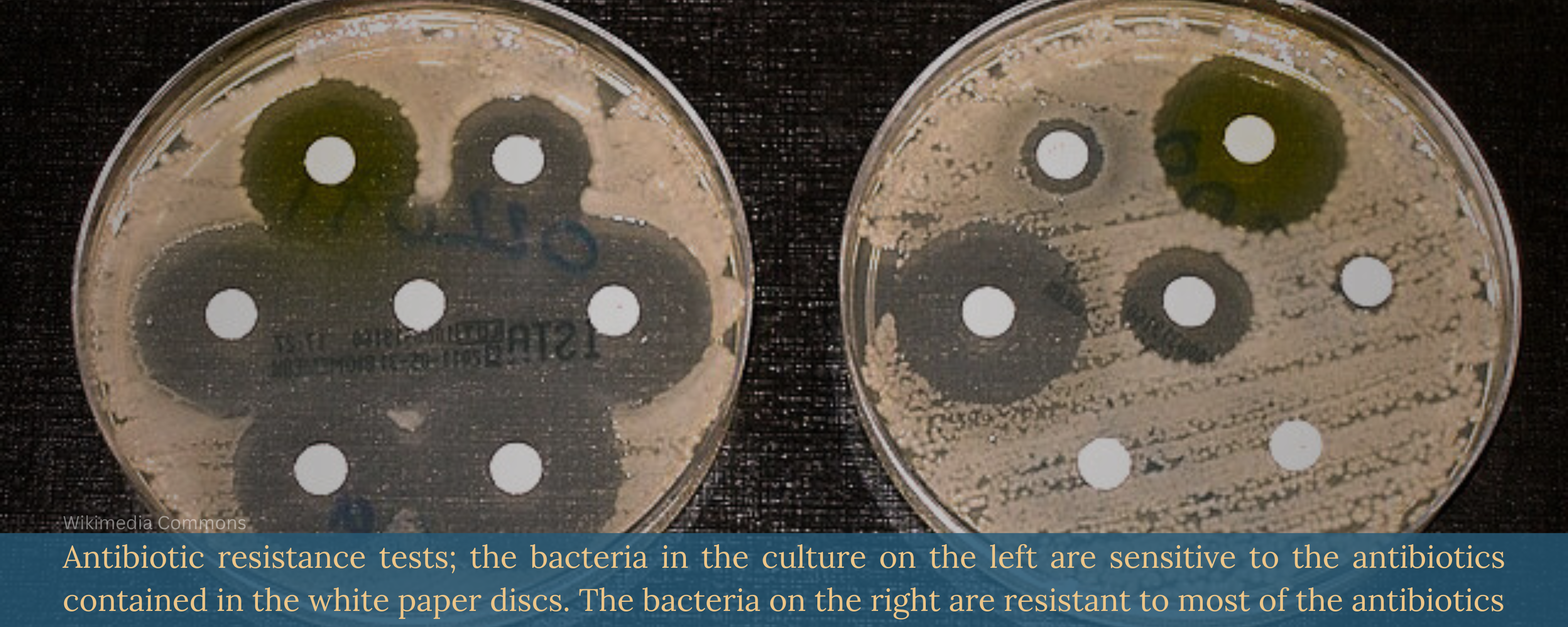
Antibiotic Resistance: The Crisis Ensues…
One of the most significant breakthroughs in the field of medicine is said to be the discovery of antibacterial therapy. However, in the year 1945, Sir Alexandar Fleming warned that the overuse or abuse of antibiotics could lead to time that would bring antibiotic resistance.
The evolution of antibiotic resistance has been driven by the overuse of antibiotics. The evolution of drug resistance in many pathogens has resulted in the current antimicrobial crisis the world is facing today. Antibiotic resistance emerges when pathogens like bacteria or other microorganisms gain the ability to resist the antibiotic or antimicrobial drug that once effectively acted on that pathogen.
Effects of Antibiotic resistance
Antibiotic resistance has individual as well as societal impacts. The antibiotics that are prescribed to one individual can affect the resistance pattern of the whole community. Once the antifungals and antibiotics lose their efficacy then the ability to treat infection with them is also lost.
The infections caused due to antibiotic-resistant bacteria are harder to treat which often results in high medical expenses, prolonged hospital stays, and an increase in mortality rates. Infections caused due to resistant strains result in up to a two-fold high rate of fatal effects. These fatal health effects can be termed as the virulence of the strain, increase in host vulnerability, and severity of the disease.
"Antibiotics are usually prescribed to treat Bacterial infections that affect various parts of the body such as the Urinary tract, Respiratory tract, Skin, Genitalia, etc. If you're prescribed antibiotics, it's important to take them EXACTLY as directed by your Physician to ensure the best chance of effectively treating the infection and minimizing the risk of antibiotic resistance."
Dr. Areez Khoza, MBBS, Delhi
Some examples of antimicrobial resistance
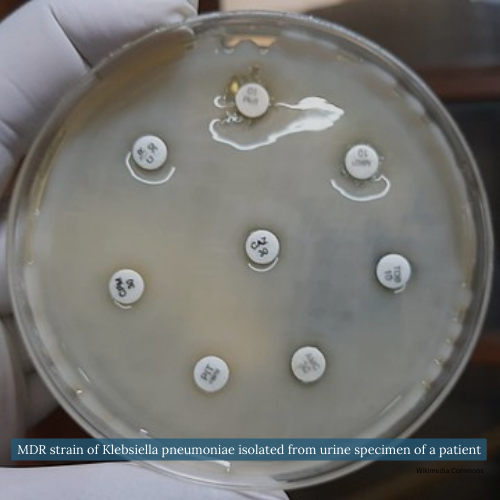
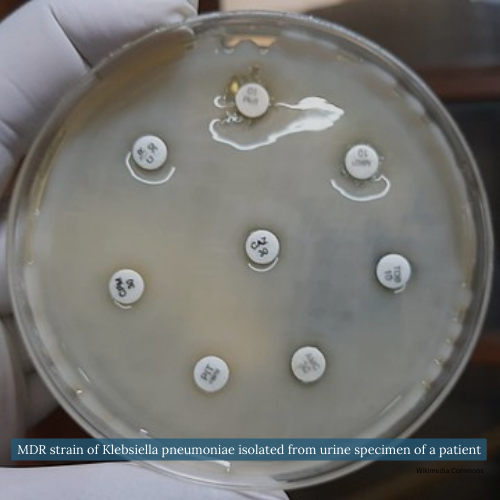
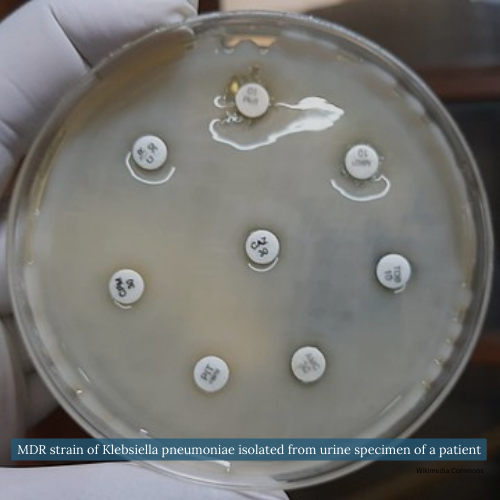
Now considered a rising threat, Carbapenem-resistant Enterobacteriaceae (CRE) is gaining attention. Carbapenem-resistant Klebsiella pneumoniae, in particular, has demonstrated a mortality risk of 2 to 5 times higher than infections caused by carbapenem-susceptible strains.
In the case of infections like gonorrhoea, Neisseria gonorrhoeae strains exhibit resistance to most antibiotics, potentially resulting in their transformation into other secondary Infections & Sexually transmitted infections, such as the Human Immunodeficiency Virus, etc. Antimicrobial resistance contributes to increased mortality rates and has the potential for the spread of other infections due to treatment limitations.
Some examples of antimicrobial resistance
Now considered a rising threat, Carbapenem-resistant Enterobacteriaceae (CRE) is gaining attention. Carbapenem-resistant Klebsiella pneumoniae, in particular, has demonstrated a mortality risk of 2 to 5 times higher than infections caused by carbapenem-susceptible strains.
In the case of infections like gonorrhoea, Neisseria gonorrhoeae strains exhibit resistance to most antibiotics, potentially resulting in their transformation into other secondary Infections & Sexually transmitted infections, such as the Human Immunodeficiency Virus, etc. Antimicrobial resistance contributes to increased mortality rates and has the potential for the spread of other infections due to treatment limitations.
Some examples of antimicrobial resistance
Now considered a rising threat, Carbapenem-resistant Enterobacteriaceae (CRE) is gaining attention. Carbapenem-resistant Klebsiella pneumoniae, in particular, has demonstrated a mortality risk of 2 to 5 times higher than infections caused by carbapenem-susceptible strains.
In the case of infections like gonorrhoea, Neisseria gonorrhoeae strains exhibit resistance to most antibiotics, potentially resulting in their transformation into other secondary Infections & Sexually transmitted infections, such as the Human Immunodeficiency Virus, etc. Antimicrobial resistance contributes to increased mortality rates and has the potential for the spread of other infections due to treatment limitations.
Causes of Antibiotic Resistance

Overuse and Abuse of Antibiotics
One of the major causes of antibiotic resistance is the overuse and abuse of antibiotics. In various Countries, there is an unregulated sale of antibiotics, and drugs are available over the counter even without prescriptions. This ability to easily access antibiotics at plentiful and cheap rates has contributed to abuse of the antibiotics.

Overuse and Abuse of Antibiotics
One of the major causes of antibiotic resistance is the overuse and abuse of antibiotics. In various Countries, there is an unregulated sale of antibiotics, and drugs are available over the counter even without prescriptions. This ability to easily access antibiotics at plentiful and cheap rates has contributed to abuse of the antibiotics.

Incorrect Prescription of Antibiotics
Incorrect prescription of antibiotics can lead to complications of antibiotic therapy. Studies reveal that at least in 30 to 50% of the cases the duration of antibiotic doses, and treatment indication is incorrect.

Incorrect Prescription of Antibiotics
Incorrect prescription of antibiotics can lead to complications of antibiotic therapy. Studies reveal that at least in 30 to 50% of the cases the duration of antibiotic doses, and treatment indication is incorrect.
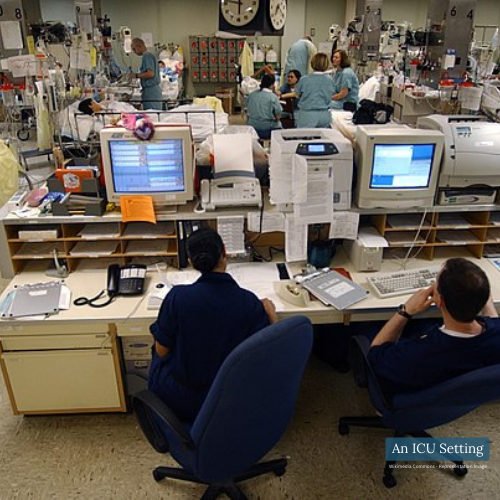
Inappropriate Antibiotic Use in ICUs
Inappropriate Antibiotic Use in ICUs: 60% of the antibiotics that are prescribed in the ICUs are proven to be of no use or inappropriate. This highlights the need for careful and targeted antibiotic usage, particularly in critical care settings
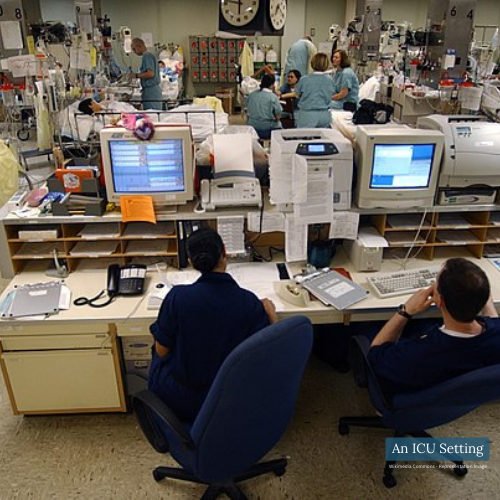
Inappropriate Antibiotic Use in ICUs
Inappropriate Antibiotic Use in ICUs: 60% of the antibiotics that are prescribed in the ICUs are proven to be of no use or inappropriate. This highlights the need for careful and targeted antibiotic usage, particularly in critical care settings

Antibiotic Use in Livestock and Ecological Implications
Antibiotics have been used in treating livestock which is then ingested by humans through food consumption. This leads to the transfer of resistant bacteria to humans using meat products. This has been known to affect the environmental microbiome as well. As the major part of antibiotics given to farm animals is excreted by them through urine and stool which spreads around as fertilizers and surface runoff. All of this promotes the exposure of antibiotics in the environment.

Antibiotic Use in Livestock and Ecological Implications
Antibiotics have been used in treating livestock which is then ingested by humans through food consumption. This leads to the transfer of resistant bacteria to humans using meat products. This has been known to affect the environmental microbiome as well. As the major part of antibiotics given to farm animals is excreted by them through urine and stool which spreads around as fertilizers and surface runoff. All of this promotes the exposure of antibiotics in the environment.
Addressing the Challenge
To combat antibiotic resistance the pharmaceutical industry has been working on developing new antibiotics. According to some studies, a decrease in the use of antibiotics can reverse the resistance to antibiotics to some extent. As there is a high necessity for the treatment of bacterial infections practically it is not possible to completely stop the use of antibiotics, but keeping it at the minimum may help achieve the control of antibiotic resistance.
For commercially available antibiotics, it is suggested to carry out pharmaco-epidemiologic trials that will monitor and analyze the occurrence of resistance. Such trials can provide valuable insights into the effectiveness and impact of these drugs. Besides these, using antibiotics rationally, and maintaining hygienic standards would also help in overcoming the crisis of antibiotic resistance.
Prevention could emerge as the definitive solution for reducing antibiotic resistance. By practising good hygiene, administering vaccinations, and implementing various preventive measures, the demand for antibiotics can be substantially diminished by averting infections altogether.

F5 - FAQs: Antibiotics & Antibiotic Resistance
F5 - FAQs: Antibiotics & Antibiotic Resistance
1) Are there severe side effects or risks associated with antibiotics?
Answer: Just like any other drug, antibiotics may also lead to side effects. So, yes, antibiotics can have side effects like abdominal pains, and allergic reactions, and they can even have potential interactions with other medications. Additionally, using antibiotics when not needed can contribute to antibiotic resistance, impacting future treatments. It’s important to take them only when necessary and under the guidance of a healthcare provider.
2) What is the link between Vaccines and Antibiotic Resistance? What role do vaccines play in preventing antibiotic resistance?
Answer: Vaccines are an essential tool in preventing infections, which can ultimately lead to less antibiotic use. By getting vaccinated, we protect ourselves from certain illnesses caused by bacteria and viruses. This, in turn, decreases the overall use of antibiotics and the potential for antibiotic resistance to develop.
3) Can I stop taking antibiotics if I start feeling better?
Answer: It is important to complete the full course of antibiotics. Stopping early might not eliminate the bacteria, allowing them to develop resistance and potentially cause a relapse that’s harder to treat. Finishing the entire antibiotic course is crucial to ensure all bacteria are eliminated and to minimise the risk of antibiotic resistance.
4) How does agriculture contribute to antibiotic resistance?
Answer: In agriculture, antibiotics are sometimes used to promote growth and prevent infections in livestock. Overuse and misuse of antibiotics in agriculture can lead to the development of antibiotic-resistant bacteria in animals. These resistant bacteria can then spread to humans through direct contact, consumption of contaminated food, or environmental contamination.
5) Can antibiotic resistance affect me even if I’ve never taken antibiotics?
Answer: Yes, antibiotic resistance can spread through the environment, food, and direct contact. If you get an infection caused by antibiotic-resistant bacteria, it might be harder to treat, regardless of your antibiotic use history. Hence, it is important to take proper care of yourself, maintain good hygiene, follow a balanced diet, avoid unprotected sexual interactions, and consult your physicians.
1) What should I do if I am prescribed antibiotics for an illness?
Answer: Antibiotics are usually prescribed to treat Bacterial infections that affect various parts of the body such as the Urinary tract, Respiratory tract, Skin, Genitalia, etc. If you’re prescribed antibiotics, it’s important to take them EXACTLY as directed by your Physician to ensure the best chance of effectively treating the infection and minimizing the risk of antibiotic resistance.
2) Are there severe side effects or risks associated with antibiotics?
Answer: Just like any other drug, antibiotics may also lead to side effects. So, yes, antibiotics can have side effects like abdominal pains, allergic reactions, and they can even have potential interactions with other medications. Additionally, using antibiotics when not needed can contribute to antibiotic resistance, impacting future treatments. It’s important to take them only when necessary and under the guidance of a healthcare provider.
3) What is the link between Vaccines and Antibiotic Resistance? What role do vaccines play in preventing antibiotic resistance?
Answer: Vaccines are an essential tool in preventing infections, which can ultimately lead to less antibiotic use. By getting vaccinated, we protect ourselves from certain illnesses caused by bacteria and viruses. This, in turn, decreases the overall use of antibiotics and the potential for antibiotic resistance to develop.
4) Can I stop taking antibiotics if I start feeling better?
Answer: It is important to complete the full course of antibiotics. Stopping early might not eliminate the bacteria, allowing them to develop resistance and potentially cause a relapse that’s harder to treat. Finishing the entire antibiotic course is crucial to ensure all bacteria are eliminated and to minimise the risk of antibiotic resistance.
5) How does agriculture contribute to antibiotic resistance?
Answer: In agriculture, antibiotics are sometimes used to promote growth and prevent infections in livestock. Overuse and misuse of antibiotics in agriculture can lead to the development of antibiotic-resistant bacteria in animals. These resistant bacteria can then spread to humans through direct contact, consumption of contaminated food, or environmental contamination.
6) Can antibiotic resistance affect me even if I’ve never taken antibiotics?
Answer: Yes, antibiotic resistance can spread through the environment, food, and direct contact. If you get an infection caused by antibiotic-resistant bacteria, it might be harder to treat, regardless of your antibiotic use history. Hence, it is important to take proper care of yourselves, maintain good hygiene, follow a balanced diet, avoid unprotected sexual interactions, and consult your physicians.
Disclaimer: The information provided in this FAQ section is meant for general informational purposes and should not be considered a replacement for professional medical advice, diagnosis, or treatment. For any concerns related to a medical condition, it is important to consult your physician. It’s important to note that medical advice, diagnosis, and treatment plans are individualized and rely on the physician’s assessment and counselling, often varying from person to person.

Author: Sanika Pande
Medically Reviewed by Dr. Darshit Patel, MD, Mumbai








