
Polyorchidism: Understanding the Rare Condition of Extra Testicles
Introduction
Polyorchidism, also known as supernumerary testis, is a rare congenital condition characterized by the presence of more than two testicles. While the most common form of this condition involves three testicles (triorchidism), variations with more than three testicles have also been documented. This anomaly is exceedingly uncommon, with fewer than 250 cases reported in medical literature. [1, 2]
Despite its rarity, understanding polyorchidism is important for recognizing and managing potential complications associated with the condition.
Causes and Development
The male reproductive system typically includes two testicles that are located within the scrotum. These testicles, also known as gonads, are responsible for producing sperm and testosterone.
The exact cause of polyorchidism is not well understood. One theory suggests that polyorchidism results from an abnormal division of the genital ridge before the 8th week of embryonic development. The genital ridge is a cluster of cells in the developing embryo that eventually forms the reproductive organs. For reasons that are still unknown, the genital ridge might divide in such a way that an additional testis forms, either in the scrotum or higher up in the inguinal region.
Polyorchidism is not typically associated with other developmental or anatomical abnormalities. There is no evident hereditary or environmental link to this rare condition. [1, 3]
Symptoms of Polyorchidism
Most individuals with polyorchidism do not exhibit symptoms and are often unaware of their condition until it is discovered incidentally during a physical examination or imaging studies conducted for other reasons. The additional testis or testes are most commonly present in the scrotum (66% of cases), inguinal canal (23% of cases), or retroperitoneum (9% of cases). The extra testicle is generally smaller than the two normal ones, which often leads to it being undetected for a long time.
In some cases, a painless mass or swelling in the scrotum may be noticed, which could be mistaken for other conditions such as a hydrocele, varicocele, or testicular tumour. [1, 3, 4]
How is polyorchidism diagnosed?
Polyorchidism is often discovered incidentally, as it typically does not present symptoms. The majority of cases were discovered incidentally during surgeries performed for other conditions such as inguinal hernia, undescended testicle, testicular torsion, or scrotal pain. Only 16% of patients reported noticing an additional mass without experiencing any symptoms. [2]
The diagnosis of polyorchidism typically involves:
- Physical Examination: A healthcare provider may detect the presence of an additional testis during a routine scrotal examination. This involves palpating the scrotum to feel for any abnormal lumps or masses. [3]
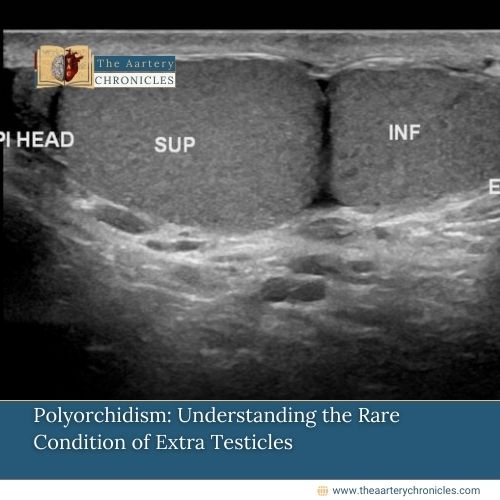
- Ultrasound: This imaging technique is commonly used to confirm the presence of extra testicular tissue. Ultrasound can help differentiate between polyorchidism and other scrotal abnormalities such as hydroceles, varicoceles, or testicular tumours. It provides detailed images of the scrotum and its contents, making it a reliable diagnostic tool. [3, 4]
- Magnetic resonance imaging (MRI): MRI is another imaging method that offers more detailed and comprehensive images than an ultrasound. It is used to accurately assess the anatomy of the scrotum and confirm the diagnosis of polyorchidism. [3, 4]
- Contrast-enhanced ultrasound (CEUS): A contrast-enhanced ultrasound (CEUS) can be an alternative to MRI for diagnosing scrotal masses. This technique involves the intravenous injection of ultrasound contrast agents containing microbubbles. Contrast-enhanced ultrasound (CEUS) is safe and well-received by patients. It is used to evaluate scrotal lesions and offers better visualization of vascularity than the color Doppler method, capable of detecting microvessels as small as 2–7 µm. [3]
These tests can accurately determine the size and location of the testes, providing crucial information such as their vascularity and any indications of testicular cancer.
Common Conditions Associated with Polyorchidism
While polyorchidism itself is generally benign and asymptomatic, some common conditions associated with it include:
- Cryptorchidism: This condition, where one or both testes fail to descend into the scrotum, is often found concurrently with polyorchidism.
- Inguinal Hernia: There is an increased incidence of inguinal hernias on the side where the supernumerary testis (extra testis) is located.
- Testicular torsion: The presence of an extra testis can potentially increase the risk of testicular torsion, a painful condition where the testis twists on the spermatic cord, cutting off blood supply.
- Testicular cancer: Although rare, individuals with polyorchidism may have a slightly higher risk of developing testicular cancer, including conditions like seminoma and intratubular germ cell neoplasia (IGCN).
- Hydrocele: This is a fluid-filled sac surrounding a testicle that can occur in cases of polyorchidism. [3]
Does polyorchidism affect fertility?
Fertility is generally not impacted by polyorchidism. For instance, a 2010 study reported a case where a father of three children discovered a painless mass in his scrotum. After undergoing imaging tests, no further treatment was required since there were no associated health concerns. An extra testicle, whether a third or fourth, may function just like a normal one. [5]
However, if you have been diagnosed with polyorchidism and are experiencing fertility issues, it is advisable to consult a fertility specialist. Although an additional testicle typically does not disrupt the function of the other two, further fertility testing may be necessary to ensure everything is functioning correctly
Treatment for Polyorchidism
Unless cancer or other complications related to the extra testicle are present, no medication or procedure is required for polyorchidism. After diagnosis, regular monitoring should be part of annual check-ups. This involves tracking any new symptoms and undergoing MRIs or ultrasounds as recommended by your doctor.
There is debate regarding whether to remove an extra testicle due to its increased cancer risk. If cancer is suspected based on testicular biopsy or imaging, then an orchiopexy (removal of the additional testicle) may be advisable. Additionally, some doctors suggest removing abdominal testicles due to their higher risk of becoming cancerous. [3, 5]
Conclusion
Polyorchidism is a rare condition that often goes unnoticed due to its lack of symptoms. While generally benign, it requires awareness and monitoring due to the slight risk of complications such as malignancy and torsion. Advances in medical imaging have made it easier to diagnose and manage this condition, allowing individuals with polyorchidism to lead healthy, normal lives. If you suspect you might have polyorchidism or have any concerns about your reproductive health, consult with a healthcare professional for proper evaluation and guidance.
- Diagnosis and Management of Polyorchidism: A Case Report and Literature Review - PMC (nih.gov)
- Polyorchidism: A Meta-Analysis | Journal of Urology (auajournals.org)
- Polyorchidism: An Up-to-Date Systematic Review - PMC (nih.gov)
- A Case Report: Triorchidism; is a Rare Mistaken Cause for Extra Testicular Neoplasm - ScienceDirect
- Management of polyorchidism: Surgery or conservative management? - PMC (nih.gov)









