Lithopedion: Understanding the Rare Condition of Stone Babies
Introduction of Lithopedion – A Medical Marvel of Stone Babies
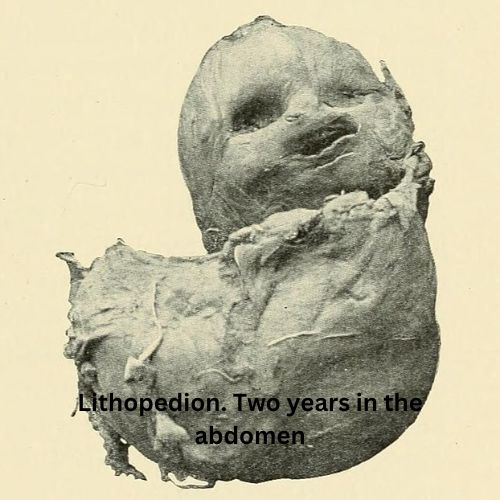
Lithopedion is a rare and extraordinary medical phenomenon in which a fetus calcifies and becomes mummified within the mother’s body, often following an ectopic pregnancy. Commonly known as a “stone baby,” the term “lithopedion” is derived from the Greek words “lithos,” meaning stone, and “paidion,” meaning child. The condition typically results from an abdominal ectopic pregnancy where the deceased fetus is not expelled, leading the body to initiate a calcification process to prevent infection.
Aetiology of Lithopedion
Ectopic Pregnancy
Lithopedion most commonly arises from an abdominal ectopic pregnancy. After fetal demise, the body cannot expel the fetal remains due to their size and location. To protect the mother from infection, the body initiates a calcification process. Over time, this process encases the dead fetal tissue in a calcified shell, a transformation that can occur over several years.
A rarer variant, lithokelyphopedion, involves the calcification of both the fetus and the amniotic sac, adding another layer of complexity to the condition.
- The mechanisms behind this dual calcification are not entirely understood but are likely an extension of the same protective processes that lead to lithopedion formation.
- The body’s ability to isolate and neutralize potentially infectious tissue is remarkable, reflecting a unique biological response to a failed ectopic pregnancy.
Clinical Presentation of Lithopedion
Patients with lithopedion may remain asymptomatic for years, with the diagnosis often occurring incidentally. In rare instances, symptoms may develop such as
- Abdominal pain
- A palpable mass
- Gastrointestinal discomfort
Lithopedion is frequently discovered during imaging studies performed for unrelated reasons, such as X-rays, ultrasounds, CT scans, or MRIs, and can be easily misdiagnosed as conditions like
- Calcified fibroids
- Ovarian dermoid cysts
- Tumors
- Gallstones
There have been rare reports of women carrying a lithopedion alongside a viable intrauterine pregnancy. This co-occurrence is exceptionally rare and presents unique challenges for both diagnosis and management, as the presence of a calcified fetus may complicate the standard monitoring and care of the concurrent viable pregnancy.
Diagnosis of lithopedion
The diagnosis of lithopedion typically relies on imaging studies.
- An X-ray can often reveal the calcified fetal structure within the abdomen.
- An ultrasound or CT scan provides more detailed imaging to confirm the diagnosis.
- Magnetic Resonance Imaging (MRI) may be used for further characterization, especially when the calcified mass is mistaken for other conditions like tumours or gallstones.
- Differentiating lithopedion from other intra-abdominal calcifications is crucial to avoid unnecessary surgical interventions.
Management of Lithopedion
Generally, asymptomatic patients with lithopedion do not require treatment. Management strategies depend on the severity of symptoms.
- If symptoms such as pain, discomfort, or complications develop, surgical removal of the calcified fetus may be necessary.
- In cases where the lithopedion is large or causes complications like bowel obstruction, surgery is typically performed to alleviate symptoms.
Most asymptomatic cases do not require surgical intervention, as lithopedion remains a medical curiosity. The encapsulated, calcified fetus typically poses no threat, and the body’s remarkable ability to adapt to such extraordinary circumstances usually prevents complications such as infection or obstruction.
Potential Complications of Lithopedion
While most cases of lithopedion are asymptomatic and benign, potential complications can arise. These may include
- Bowel obstruction
- Infection
- Pressure effects on adjacent organs, depending on the size and location of the lithopedion.
- Rarely, if the calcified mass erodes into the gastrointestinal tract or urinary system, it can cause symptoms necessitating prompt medical intervention, like
- Bleeding
- Infection
- Fistula formation
Follow-Ups of Lithopedion
For patients who do not undergo surgery, regular follow-up is essential to monitor the lithopedion for any changes in size or position that could potentially lead to complications. Follow-up care typically involves
- Periodic imaging studies, such as ultrasounds or CT scans, to monitor for any changes in the lithopedion’s size or position.
- Additionally, patients should receive appropriate support and counseling to address any mental health concerns associated with the condition. The psychological impact of carrying a calcified fetus can be significant, and counseling or support groups may help patients cope with any emotional or psychological challenges.
Conclusion
Lithopedion, a rare medical condition, epitomizes the body’s remarkable ability to protect itself in extraordinary circumstances. The resilience of maternal physiology in such cases is a profound medical curiosity. As medical science continues to explore the mysteries of rare conditions like lithopedion, it will undoubtedly remain a testament to the complexities and intricacies of human biology. Continued research into lithopedion could lead to a better understanding of ectopic pregnancies and potential improvements in diagnosis, management, and patient support.
- Kumar, P., & Clark, M. (2020). Kumar and Clark’s Clinical Medicine (10th ed.). Elsevier.
- Cunningham, F. G., Leveno, K. J., Bloom, S. L., Dashe, J. S., Hoffman, B. L., & Spong, C. Y. (2018). Williams Obstetrics (25th ed.). McGraw-Hill Education.
- Buletti, C., et al. (2011). Ectopic pregnancy. Medical Journal of Obstetrics and Gynecology, 58(2), 135-141.