Anaemia in Pregnancy: Causes, Symptoms, and Management
Introduction
Anemia is a prevalent condition among pregnant women. It frequently occurs when an increase in blood volume leads to a lower concentration of red blood cells and impairs oxygen delivery. [1]
Anemia is a condition in which the body lacks enough healthy red blood cells or hemoglobin to carry adequate oxygen to its tissues.
Anemia during pregnancy can increase the risk of premature birth, low birth weight, foetal malformation, and even maternal mortality. Learning about the different types of anemia, their common symptoms, and available treatments can help pregnant women and lactating mothers identify the warning signs and prevent complications.
What causes anemia during pregnancy?
Although mild anemia is common during pregnancy, it can escalate into a serious issue necessitating advanced medical intervention if left untreated. Physiological anemia, known as dilutional anemia, is a natural occurrence in pregnancy. As blood volume increases, the plasma volume increases more significantly, resulting in a lower concentration of red blood cells. However, various other types of anemia with distinct causes can manifest during pregnancy. This includes:
1. Iron-deficiency Anemia: Due to lack of iron
Pregnancy significantly increases the body’s need for iron. This is because the mother’s blood volume increases substantially by 45% to support the growing foetus and placenta. Additionally, the mother’s body supplies iron required for the baby to produce their own hemoglobin. While this supports better oxygen and nutrient transport, it also raises the demand for minerals like iron, potentially leading to reduced hemoglobin production or iron deficiency. [2, 3]
2. Folate deficiency Anemia: Due to lack of folate
Folate-deficiency anemia is another prevalent type of anemia observed during pregnancy due to the increased folate requirements. Folate, a water-soluble vitamin, plays a crucial role in preventing neural tube defects or cognitive brain issues in pregnancy. [4]
3. Vitamin B12 deficiency: Due to lack of vitamin B12
Vitamin B12 is essential for red blood cell production and is primarily sourced from fortified foods, meat, fish, poultry, and eggs. Consequently, individuals, particularly females assigned at birth (FAAB) who are vegans or vegetarians and don’t regularly consume these foods, may face an increased risk of deficiency. Folate and vitamin B12 deficiencies frequently coincide. [1, 5]
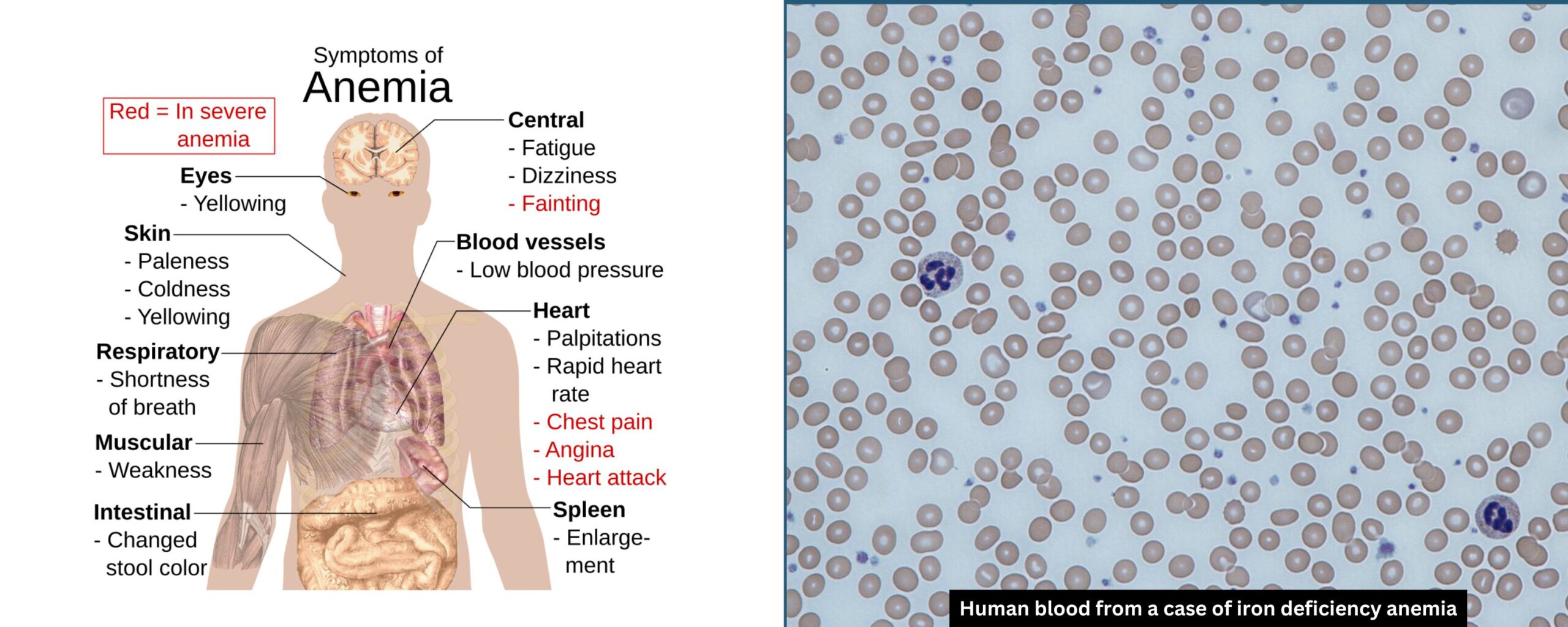
What are the signs and symptoms of anemia during pregnancy?
Anemia can present with a variety of symptoms, some of which might be mistaken for normal pregnancy-related changes. Common symptoms include:
- Fatigue or weakness
- Pale or yellowish skin
- Shortness of breath
- Dizziness or light-headedness
- Reduced body temperature
- Headaches
- Heart palpitations
- Restless leg syndrome (unintended movement in the lower limbs) [1, 2]
During lactation, these symptoms can persist or worsen if iron levels are not adequately restored.
Who is at an increased risk for anemia during pregnancy?
During pregnancy, blood volume increases by 20% to 30%, requiring more iron for additional red blood cells. A woman may be at a higher risk for anemia if she is:
- Expecting multiples
- Not consuming sufficient iron
- Having pregnancies close together
- Experiencing heavy menstrual bleeding before pregnancy
- Frequently vomiting due to morning sickness [1]
How is anemia diagnosed during pregnancy?
Anemia can be diagnosed with a complete blood count (CBC), a blood test often conducted during one of the initial prenatal visits.
The healthcare provider uses the CBC to examine:
- The number, size, and shape of red blood cells can indicate conditions like sickle cell anemia
- The amount of iron stored in the body
- Levels of vitamins B12 and B9 in the body
The doctor may then request additional tests to identify if there is another type of anemia or an underlying medical condition. [1]
Severe anemia is diagnosed when a CBC reveals hemoglobin levels of 6.5 to 7.9 grams per deciliter (g/dL).
Management and Preventive Measures
Severe anemia during pregnancy is typically treated with blood transfusions. However, mild anemia during pregnancy is preventable with a nutrition rich diet. Some tips that ensure pregnant women get the essential vitamins and minerals to maintain red blood cells within the range include the following:
- Iron Supplements: Oral iron supplements are commonly prescribed to treat anemia. In severe cases, intravenous iron or blood transfusions might be necessary.
- Folate and Vitamin B12 Supplements: Supplementation is crucial, particularly if deficiencies are detected. These essential nutrients are commonly found in prenatal supplements.
- Dietary Modifications: Consuming iron-rich foods such as lean meats, leafy green vegetables, legumes, and iron-fortified cereals can help increase iron intake. Foods rich in vitamin C, like citrus fruits, can enhance the absorption of iron in the blood.
- Frequent Monitoring: Frequent blood tests during and after pregnancy help track the effectiveness of treatment and ensure that anemia is being properly managed.
- Addressing the Underlying Condition: If anemia is caused by an underlying health condition, it is important to manage that condition with appropriate medical care.
To prevent anemia, it’s advisable to consume a minimum of 30 milligrams (equivalent to three servings) of iron daily through diet. If achieving this through dietary means is challenging, it’s recommended to discuss with your healthcare provider the possibility of taking an iron supplement. [1]
Complications of untreated anemia during pregnancy
If left untreated, anemia can worsen over time. Insufficient oxygen in the blood can harm the organs and strain the heart, leading to:
- Heart failure
- Irregular heartbeat (arrhythmia)
- Enlarged heart [1]
Four Frequently Asked Questions
1. What is the impact of anemia on the baby during pregnancy?
The developing foetus depends on the mother to obtain sufficient iron, vitamin B12, and folic acid. Anemia can impact foetal growth, particularly in the first trimester. If left untreated, anemia increases the risk of your baby being born with anemia, which can cause developmental issues. Additionally, it raises the chances of preterm delivery and having a low-birth-weight baby. [1]
2. Can anemia during pregnancy cause miscarriage?
No, anemia during pregnancy doesn’t directly lead to miscarriage, but severe anemia can result in pregnancy complications. [1]
3. In what trimester of pregnancy does anemia develop?
Research indicates that over 90% of cases of pregnancy-related anemia occur during the third trimester. [6]
4. Is anemia during pregnancy a normal occurrence?
Yes. Due to the increased blood volume during pregnancy, experiencing mild anemia is common. Iron deficiency is prevalent among pregnant women, with up to 52% of women in developing countries not meeting their iron requirements. Severe anemia, on the other hand, is uncommon. Nevertheless, both mild and severe cases of anemia necessitate treatment to safeguard the health of both the mother and the foetus. [1]
Conclusion
Anemia in pregnant women is a common but manageable condition. Through proper dietary measures, supplementation, and regular medical check-ups, the risks associated with anemia can be significantly reduced. Healthcare providers play a vital role in educating and supporting women during pregnancy to ensure optimal health outcomes for both mother and baby. Recognizing and addressing anemia early can lead to healthier pregnancies and better developmental outcomes for newborns.
- Anemia During Pregnancy: Symptoms, Risks & Prevention (clevelandclinic.org)
- Anemia and Pregnancy - Hematology.org
- Physiological changes in pregnancy - PMC (nih.gov)
- Folate-Deficiency Anemia | Johns Hopkins Medicine
- Vitamin B12 - Health Professional Fact Sheet (nih.gov)
- Study on types of anaemia and foetomaternal outcome in antenatal patients - PMC (nih.gov)









