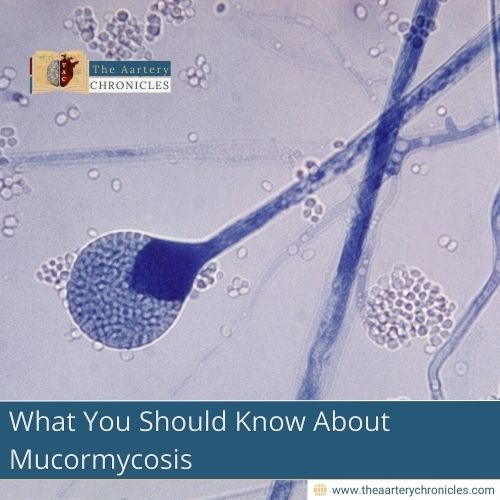

What You Should Know About Mucormycosis
Introduction
Mucormycosis or zygomycosis is a rare but chronic infection of the lungs, brain or sinuses and typically occurs in people with a poor immune system
Causes
Mucormycosis is caused by a group of fungi called mucoromycetes. These fungi are mainly found in decaying organic matter, including spoiled bread, vegetables, and fruits, as well as compost piles and soil. People are most likely to come into contact with the fungus through environmental exposure.
People with weak immune systems are more likely to get infected. These include people with conditions such as:
- Diabetes
- AIDS
- Long-term usage of steroids
- Metabolic acidosis
- Poor nutrition
- Lymphoma and Leukaemia
- Burns
- Stem cell or organ transplant
- People using immunomodulating drugs, such as the antifungal voriconazole, may also be at risk.
Transmission
- It is non-contagious and is not transmitted through direct touch between people.
- This fungus is present in the environment. Spores from the environment can be transmitted by inhalation, inoculation, or ingestion.
- Although the majority of instances are rare, healthcare-related outbreaks have been connected to adhesive bandages, wooden tongue depressors, hospital linens, etc.
- It primarily affects the sinuses or lungs after inhalation of fungal spores from the air, and in some cases, the infection may spread to the brain and eyes. It can also occur on the skin when a cut, burn, or other injury becomes infected.
Disease burden
- The global rate of incidence of mucormycosis ranges between 005 and 1.7 per million population
- The prevalence of mucormycosis in India is estimated to be 140 per million population
- A meta-analysis and systemic review of 851 case reports was published in 2018, which revealed that 389/851 (46%) of patients died
- The Fatality rate was high, around 68% among the patients with disseminated mucormycosis and low (31%) in individuals with cutaneous disease.
Types And Symptoms
The symptoms of mucormycosis are highly dependent on the location of the infection within the body. However, sinusitis or sinus infection is the most common, which involves nasal congestion, sinus pain, etc. Fever and headache may also be experienced.
|
|
| · Facial swelling · Nasal congestion · Fever · Headache · Lesions on the upper side of the mouth or the nasal bridge |
| · Pain in the chest · Shortness of breath · Cough · Fever |
| · Skin lesions · Darkening of the infected areas · Redness, swelling and pain around the wound
|
| · Nausea · Vomiting · Pain in the abdomen |
|
|
Diagnosis
- Early diagnosis and administration of appropriate treatment are essential to improve the outcomes of individuals with mucormycosis.
- Some of the common diagnostic methods involve fungal staining and tissue biopsy.
- Endobronchial ultrasound is a specialised form of bronchoscopy. A healthcare provider uses a thin, flexible tube with light and an ultrasound to capture images from inside the lungs.
- Imaging tests, including chest X-rays, MRI and CT scans of sinuses, lungs or other body parts, may also be employed to support the diagnosis.
Management and Treatment
- Antifungal medications are used for the treatment of mucormycosis.
- Surgical excision may also be needed to remove dead or infected tissue
- Some antifungal medications that are commonly used for treating mucormycosis include:
- Amphotericin B
- Posaconazole
- Isavuconazole
- The overall prognosis is determined by many factors, such as the infection site, rapidity of diagnosis, treatment, degree of immunosuppression and the pre-existing medical conditions of the patient.
- Approximately 50% of the case fatality is recorded for the disease, however, early diagnosis and treatment can result in better outcomes.
Preventing Mucormycosis
- It is important to consult your physician to determine the risk of infection if your occupation involves exposure to fungi
- Limit spending time in areas with dirt or dust, such as sites of construction, wear protective respirators and other gear to avoid inhalation of spores
- Avoid digging and other activities that could potentially disrupt the soil and release spores. If the work is necessary, use protective covering such as gloves.
- Keep cuts and abrasions clean to avoid infection.