Cardiac Asthma Explained: What Your Heart Is Telling You
Introduction
Cardiac asthma is a condition characterized by breathing difficulties manifested as sudden shortness of breath, often accompanied by wheezing and coughing, caused by heart failure. Despite its name, cardiac asthma is not a form of bronchial asthma, but a heart-related condition. This condition results from fluid accumulation in the lungs (pulmonary edema), which can occur when the heart is unable to pump blood efficiently. In this article, we’ll explore the symptoms of cardiac asthma, its causes, and available treatments.
What Is Cardiac Asthma?
Cardiac asthma is a type of dyspnea (difficulty breathing) resulting from heart problems, usually associated with congestive heart failure. When the heart is unable to pump blood adequately, blood accumulates in the lungs, causing congestion of the lung tissue and the passage of fluid into the lungs. This causes symptoms similar to bronchial asthma, such as wheezing and a feeling of suffocation.
Cardiac asthma occurs mainly at night, when a person is lying down, since the supine position increases central venous pressure, facilitating the accumulation of fluid in the lungs.
Symptoms Of Cardiac Asthma
Symptoms of cardiac asthma can develop suddenly and quickly become severe. The condition is often confused with bronchial asthma due to similar respiratory symptoms, but the underlying cause is related to the heart, not the bronchi. The main symptoms include:
1. Severe shortness of breath (dyspnea)
Dyspnea is one of the most common and worrying symptoms of cardiac asthma. Affected individuals may experience sudden, severe shortness of breath, especially at night. This symptom is the result of fluid accumulation in the lungs, which hinders normal breathing.
Paroxysmal nocturnal dyspnea is a severe form of dyspnea that occurs suddenly during sleep and forces the patient to wake up, often trying to breathe easier by sitting up or getting out of bed. This attack can last from a few minutes to several hours.
2. Wheezing
Another common symptom is wheezing, a whistling sound heard during breathing, especially when exhaling. This symptom, characteristic of bronchial asthma, can also be present in cardiac asthma due to fluid accumulation in the lungs, which obstructs the normal passage of air.
3. Persistent cough
People with cardiac asthma may develop a dry, persistent cough, especially when lying down. In some cases, the cough may become more severe and produce frothy or pink sputum, a sign of fluid in the lungs.
4. Feeling of suffocation
During a cardiac asthma attack, patients often describe a feeling of suffocation or “being unable to breathe.” This symptom can be very frightening and may prompt the patient to immediately seek a more upright position to relieve the discomfort.
5. Increased heart rate (tachycardia)
During a cardiac asthma attack, patients often describe a feeling of suffocation or “being unable to breathe.” This symptom can be very frightening and may prompt the patient to immediately seek a more upright position to relieve the discomfort.
6. Anxiety and agitation
The sensation of suffocation and difficulty breathing can cause severe anxiety and agitation in patients. This emotional reaction is understandable and common in those experiencing a cardiac asthma attack, as the inability to breathe properly can be extremely distressing.
7. Swelling of the lower limbs (peripheral edema)
In patients with cardiac asthma, swelling of the legs and ankles is also common. This swelling (peripheral edema) is due to the heart’s inability to pump blood effectively, causing fluid to accumulate in the body’s tissues, especially in the lower extremities.
Causes Of Cardiac Asthma
Cardiac asthma is almost always associated with cardiac dysfunction, particularly congestive heart failure. Some of the main causes include:
1. Left heart failure
Left-sided heart failure is a condition in which the left side of the heart fails to pump blood efficiently throughout the body. As a result, blood pools in the lungs, causing congestion and fluid buildup that leads to the symptoms of cardiac asthma.
2. High blood pressure
Hypertension (high blood pressure) is a major cause of heart failure. Prolonged elevated blood pressure can damage the heart and impair its ability to pump blood, leading to cardiac asthma.
3. Heart valve diseases
Heart valve diseases, such as mitral stenosis or mitral regurgitation, can cause blood to pool in the heart and lungs. These conditions can increase the risk of developing cardiac asthma.
4. Cardiomyopathy
Cardiomyopathies are diseases that affect the heart muscle and impair its function. People with cardiomyopathy can develop heart failure, which in turn can lead to cardiac asthma.
5. Myocardial infarction
A heart attack can damage the heart muscle and reduce its ability to pump blood efficiently. In some cases, this can lead to pulmonary edema and cardiac asthma.
Diagnosis Of Cardiac Asthma
The diagnosis of cardiac asthma is made by the doctor on the basis of symptoms, a physical examination and diagnostic tests, including:
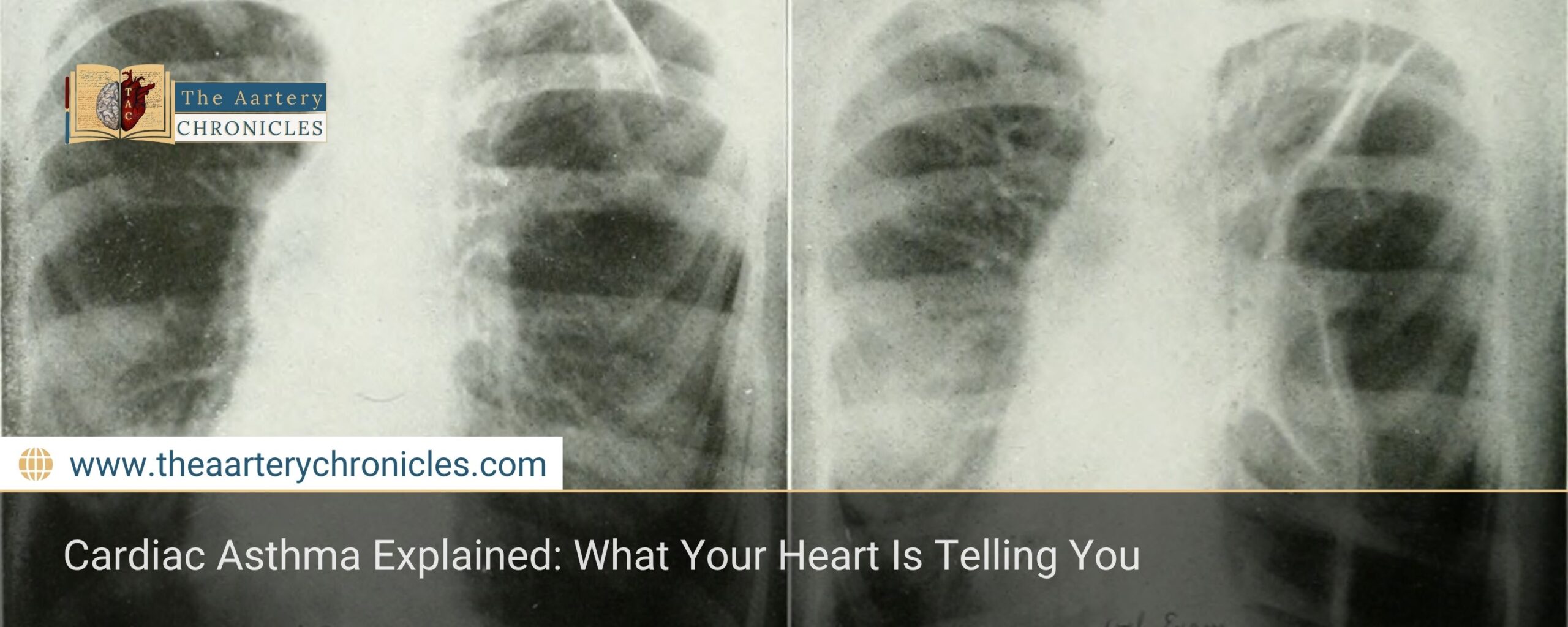
- Chest X-ray: To evaluate the presence of fluid in the lungs.
- Electrocardiogram (ECG): To monitor the electrical activity of the heart and identify any heart problems.
- Echocardiogram: To evaluate heart function and identify valve problems or other abnormalities.
- Blood tests: To measure levels of natriuretic peptides (BNP), which increase in heart failure.
Treatment Of Cardiac Asthma
Treatment of cardiac asthma focuses on managing heart failure and reducing fluid in the lungs. Treatment options include:
- Diuretics: Diuretics are drugs that help eliminate excess fluid from the body, thereby reducing lung congestion and improving breathing.
- Heart medications: Drugs such as ACE inhibitors, beta-blockers, and digitalis can be used to improve heart function and reduce pressure on the heart.
- Oxygen therapy: In severe cases, oxygen therapy may be necessary to increase the amount of oxygen available in the blood and relieve respiratory symptoms.
- Lifestyle changes: Patients with cardiac asthma should adopt a healthy lifestyle, including a balanced diet, moderate physical activity, and stress management. Avoiding smoking and limiting alcohol consumption can reduce the risk of worsening the condition.
Conclusion
Addressing cardiac asthma symptoms early and managing underlying heart conditions can significantly improve quality of life and prevent complications.