
Exploring Xenotransplantation: History, Advances, and Ethical Considerations
Abstract
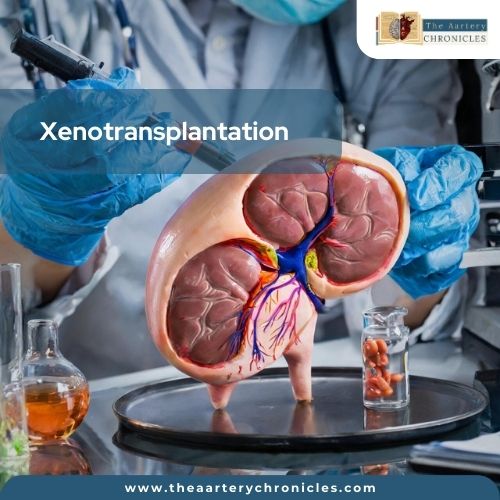
Xenotransplantation or heterologous transplantation refers to transplanting living tissues, organs, or cells from one species to another.
‘Xenotransplantation’ is derived from the Greek word ‘xenos’ which translates to foreign or strange. This method is usually used in creating human-animal chimeras, wherein a subset of animal cells is given to the human.
Xenotransplantation holds promising potential in addressing the crisis of organ shortage for transplants, as there are several successful animal-human transplants recorded. Along with its remarkable potential, many ethical and scientific challenges surround the advancement.
The Legends, and the History of Xenotransplantation
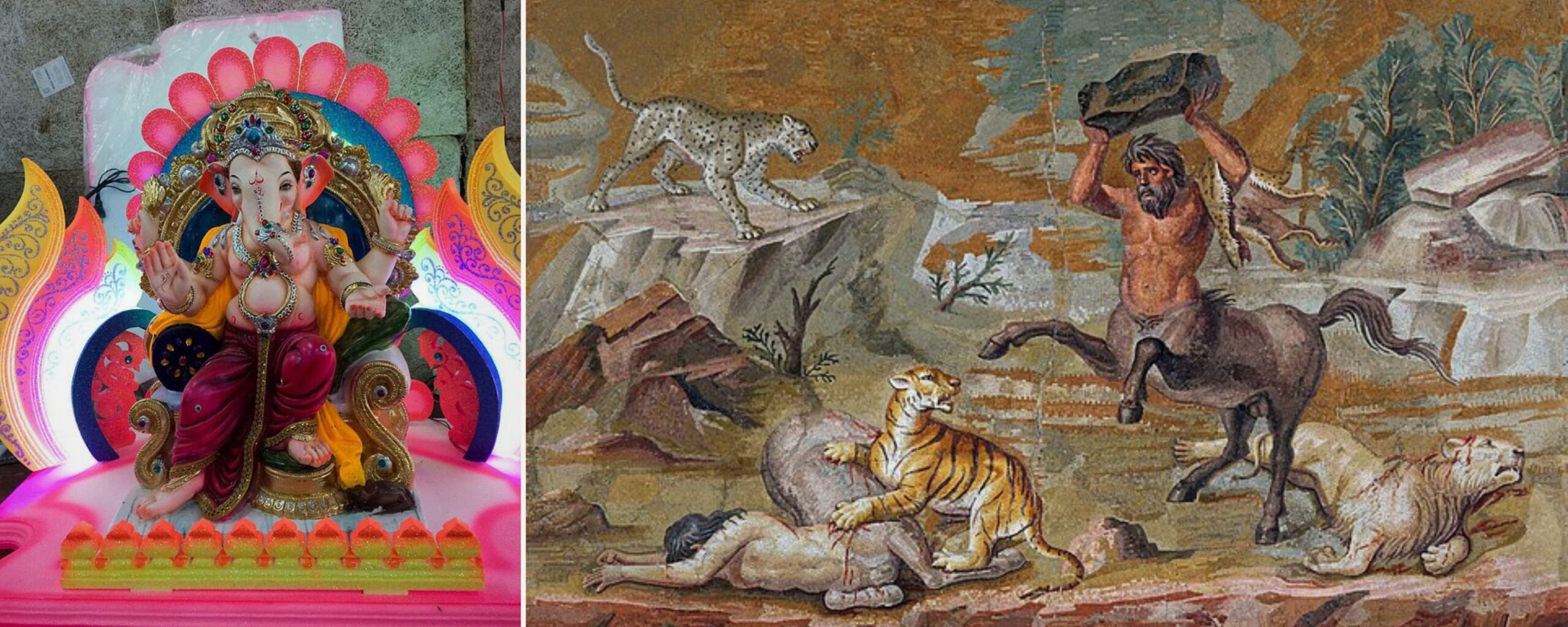
The concept of using animal organs to save human lives has a cultural and deep-rooted traditional relevance associated with numerous Hindu Puranas, related stories, and legends.
One of the most popular examples is that of the beloved God Ganesha. According to the legend, lord Ganesh was given the head of an elephant after a traumatic beheading. In Greek mythology as well, there are numerous chimeric figures including centaurs that have human torsos and minotaurs with the head of the bull. [1] One of the earliest reports of Xenotransplantation can be traced to early India around 600 BC when an Indian surgeon Sushruta used skin flaps on cut-off noses. [2]
The foundation of organ transplantation was laid by Mathieu Jaboulay and Alexis Carrel when they pioneered the technique of vascular anastomosis. Multiple attempts at xenotransplantation were made in the 20th century specifically with non-human primates including chimpanzees, baboons, and mammals such as sheep, pigs, and rabbits. [2]
Early attempts at Xenotransplantation
- The first kidney xenotransplantation in human recipients was noted in 1905 when Princeteau used pieces from rabbit kidney tissue for a child with renal failure. Unfortunately, the child died in 16 days because of pulmonary complications. [3]
- The first true xenotransplantation (at the time it was referred to as heterotransplantation) experiment, is reported to be in 1906 when Mathieu Jaboulay used a goat kidney for a 50-year nephrectomized woman. However, it had to be removed after 3 days due to thrombosis. [4]
- The first corneal transplantation was performed on a patient with pig’s cornea in 1838 and was believed to be remarkably successful. [5]
- Peter Gorer in 1961 recommended the replacement of the term heterotransplantation with xenotransplantation when he referred to a transplant between a recipient and donor coming from different species. [4]
Numerous other attempts associated with early transplantation led to failure primarily due to the absence of immunosuppression. [4]
- The longest survival rate noted for xenotransplantation was that of a 23-year-old school teacher transplanted with a chimpanzee kidney who survived without rejection but died due to electrolyte imbalance. [4]
- In the year 1984, Baby Fae was considered one of the most famous instances in the journey of xenotransplantation where a 12-day-old baby named Fae with hypoplastic left-heart syndrome acquired an ABO-mismatched baboon heart. But Baby Fae died of rejection, 20 days after surgery. [4]
These were a few significant early attempts at xenotransplantation.
Quest for the control of rejection
- Human donors were preferred to reduce the risk of rejection and due to the initial success of allotransplantations, the availability of human organs started becoming insufficient.
- To prevent xenograft rejection various strategies were explored including immune modulation, genetic manipulation, and immunosuppression.
Genetic manipulation
In recent decades tissues from pigs have been used in various applications such as bladder repair, burns, and plastic surgeries. [6] The use of genetically engineered pigs has significantly reduced the immunological barriers to xenotransplantation. Hyperacute and acute cellular rejection have been highly eliminated.
Advancements including CRISPR-Cas-9, transcription activator-like effector nuclease (TALEN), and Zinc finger nuclease have facilitated the creation of appropriate donor organs specifically genetically modified animal organs. [7]

- In 2022, the first genetically engineered pig heart was used for transplant for a human recipient with 10 genetic modifications. However, the patient died within 2 months after the surgery. [7]
- In 2024, the first successful xenotransplantation with genetically engineered organisms was performed for a 62-year-old man with renal failure. A human received a genetically modified pig kidney. CRISPR-Cas9 was used to edit the genome by the scientists from eGenesis. A total of 69 genes were modified and deletion of 3 genes. Along with these 7 human genes were added with 59 other modifications to reduce the risk of rejection. [8]
Ethical considerations
One of the most long-standing issues in the field of medicine is probably the problem of organ shortage. Due to the scarcity of organs, there has been a rise in moral obligation to increase the longevity of donated organs and use them where there is most need. [9]
The use of Genetically engineered organisms is proposed as a potential solution to the problem of organ shortage. However, it is important to consider ethical aspects at the same time. The ethical issues are diverse and multifaceted such as the increased risk of zoonotic disease, transformation of transplanted organs into cancer, etc. A few other aspects that must be taken into account are animal rights, resource allocation, and consent for xenotransplants. There have also been ethical concerns over the genetic manipulation of animals to make them suitable for transplant. Some surgeons and ethicists argue that the exaggeration of xenotransplants will reduce the human organs being donated. [10]
The promise of the future
The future holds immense levels of advancements and promise of potentially addressing the shortage of organs. With immunosuppressive therapies and innovative gene editing techniques, xenotransplantation has moved closer to being a feasible alternative for organ transplants. [11]
In conclusion, the future of xenotransplantation is defined by extensive research technological improvements, and a rising international interest in transforming these discoveries into clinical therapies.
- Evolution of Xenotransplantation as an Alternative to Shortage of Donors in Heart Transplantation | NCBI
- A Brief History of Xenotransplantation | The Annals of Thoracic Surgery
- The history of cardiac xenotransplantation: early attempts, major advances, and current progress | Frontiers
- History of xenotransplantation | PubMed
- A brief history of cross-species organ transplantation | NCBI
- Genetically Engineered Pigs for Xenotransplantation: Hopes and Challenges | NCBI
- First pig-to-human heart transplantation | NCBI
- First pig liver transplanted into a person lasts for 10 days | nature.com
- Ethical Solutions to the Problem of Organ Shortage | Cambridge.org
- Xenotransplantation: Science, Ethics, and Public Policy | NCBI
- The Future of Xenotransplantation | NCBI

Author: Ms Sanika Pande
- Biotechnology