Everything You Need to Know About Chronic Kidney Disease (CKD)
Overview
What is a chronic kidney disease?
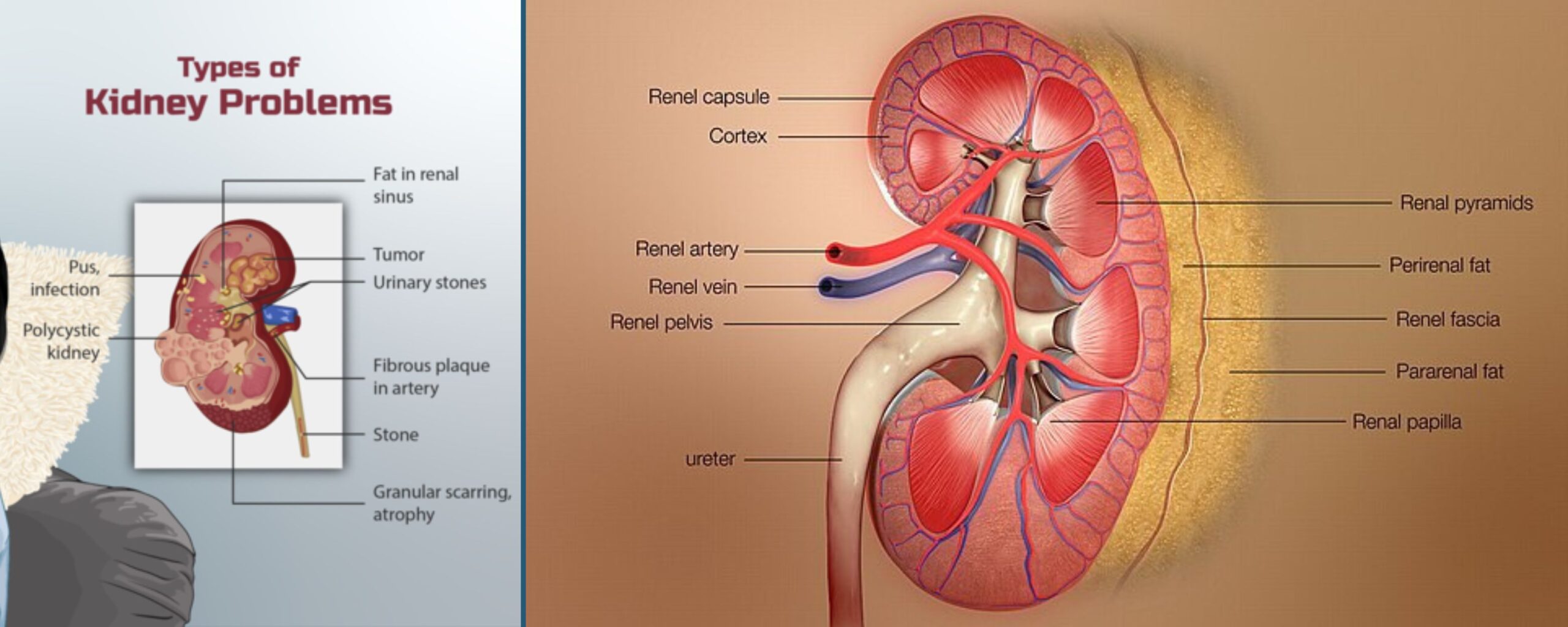
Chronic kidney disease (CKD), also known as chronic renal disease, is characterized by progressive permanent loss of kidney function over time. Kidneys are vital for overall body function as they filter waste, toxins, and excess water from the body. The waste and excess water filtered by the kidney become urine, which then travels through the ureters to be stored in the urinary bladder until it is expelled through urination. When kidneys are damaged, they cannot effectively filter waste from the body, leading to the accumulation of toxins and causing various health problems. [1]
Initially, kidney disease is asymptomatic. Symptoms usually do not manifest until significant kidney damage has occurred. Many individuals remain symptom-free until their kidney disease is at an advanced stage. The only way to diagnose kidney disease early is through blood and urine tests. [1]
This article outlines the causes and risk factors of CKD, its symptoms, effective treatment strategies, and common myths about the condition that persist in society.
Stages of Chronic Kidney Disease
Chronic kidney disease is classified into five stages depending on the glomerulation filtration rate (GFR) levels.
Glomerular Filtration Rate (GFR)
GFR is an essential measure of kidney function. It indicates how well the kidneys are filtering blood by estimating the amount of blood that passes through the glomeruli each minute. The glomeruli are the filtering units inside the kidneys that remove waste products and excess substances from the blood, which are then excreted in urine. GFR is expressed in milliliters per minute (mL/min) and is a key indicator to diagnose and monitor the progression of CKD. A healthy GFR is typically above 90 mL/min, but it can vary based on age, sex, and body size.
The stages of CKD that are classified based on GFR levels are as follows:
- Stage 1 CKD: GFR ≥ 90 mL/min indicates mild kidney damage (e.g., protein in the urine).
- Stage 2 CKD: GFR 60-89 mL/min indicates mild kidney damage and less optimal kidney function.
- Stage 3 CKD: GFR 30-59 mL/min indicates moderate kidney damage with an initial presentation of CKD symptoms.
- Stage 4 CKD: GFR 15-29 mL/min indicates severe kidney damage.
- Stage 5 CKD: GFR < 15 mL/min indicates kidney failure or end-stage renal disease (ESRD). [2, 3]
What are the symptoms of chronic kidney disease?
In the initial stages, individuals with CKD often present no symptoms. Since the loss of kidney function happens gradually, the signs and symptoms manifest overtime. Kidney damage can result in fluid buildup, waste accumulation, or electrolyte imbalances in the body. Depending on its severity, the symptoms can include:
- Fatigue and weakness
- Swelling in the legs, ankles, feet, hands, or face (edema)
- Muscle cramps
- Nausea and vomiting
- Ammonia breath (metallic taste in the mouth)
- Increase or decrease in urination frequency
- Foamy urine
- Severe skin rash or itching
- Loss of appetite
- Shortness of breath (in cases of fluid buildup in the lungs)
- Chest pain (in the case of fluid buildup around the lining of the heart)
Symptoms of kidney disease are frequently vague and non-specific and can be caused by other health conditions. Since the kidneys can compensate for reduced function, symptoms may not appear until permanent damage has been done. [1, 4]
Causes and Risk Factors
What are the causes of chronic kidney disease?
Causes of chronic kidney disease can differ globally. It mostly results from various underlying conditions, including:
- Diabetes: Diabetes is the primary cause of chronic kidney disease. Nearly one in three individuals with diabetes has chronic kidney disease.
- Hypertension: Hypertension (high blood pressure) is the second leading cause of chronic kidney disease. Nearly one in five individuals with diabetes has chronic kidney disease.
- Primary Glomerulonephritis: This is the type of kidney disease that causes inflammation of the kidney’s filtering units (glomeruli) and can lead to CKD.
- Polycystic kidney disease: This is a genetic disorder characterized by growth of fluid-filled sacs inside the kidney and can result in a gradual reduction of kidney function.
- Intestinal Nephritis: This condition refers to inflammation in kidney tubules that filter the blood.
- Pyelonephritis: This refers to recurrent kidney infections, which can result in scarring and damage to kidney tissues. [2, 4, 5]
What are the risk factors for chronic kidney disease?
Anyone can develop chronic kidney disease, but certain factors increase your risk, including:
- Diabetes (high blood sugar)
- Hypertension (high blood pressure)
- Cardiovascular (heart) disease
- Family history of kidney disease
- Abnormal kidney size or structure
- Old age (being over 60 years old)
- Obesity
- Smoking
- Frequent and a long history of using NSAID (nonsteroidal anti-inflammatory drugs) pain relievers, including over-the-counter and some prescription pain medications.
Research indicates that while chronic kidney disease (CKD) is more prevalent among women, men are more likely to progress to kidney failure sooner than women. [2, 5, 6]
Treatment and Management for Chronic Kidney Disease
While there is no cure for CKD to date, the treatment approach focuses on managing symptoms, slowing the progression of the disease, and addressing underlying causes. Key management strategies include:
Medications for Chronic Kidney Disease
- Doctors commonly prescribe ACE inhibitors or ARBs to protect the kidneys and manage hypertension.
- When the kidneys cannot remove excess phosphate, phosphate binders are used to help control phosphate levels and prevent complications like bone disease.
- Diuretics help the body eliminate excess fluid, which can reduce swelling and lower blood pressure.
- Cholesterol-lowering medications are prescribed to manage cholesterol levels and reduce cardiovascular risk, which is heightened in CKD patients.
- Doctors may prescribe erythropoietin to stimulate red blood cell production in patients with anaemia.
- Doctors often recommend vitamin D and calcitriol to prevent bone loss associated with kidney disease. [2]
Kidney Dialysis
For patients with advanced CKD or ESKD, dialysis becomes necessary to perform the kidneys’ filtering functions:
- Hemodialysis: This procedure uses a machine to filter out waste products and excess water from the blood, after which the filtered blood is returned back to the body. This procedure is usually performed for four hours a day, three times a week.
- Peritoneal dialysis: This method uses the lining of the abdomen to filter blood inside the body, and it can be done at home. [2, 4]
Kidney Transplant
In a kidney transplant, doctors replace the damaged kidney with a healthy one. They can perform the procedure using kidneys from either living or deceased donors. Living donors are typically family members, partners, or friends, as a person can lead a healthy life with just one functioning kidney. Kidneys from deceased donors usually come from individuals who have registered as organ donors. All potential donors undergo screening to ensure a suitable match and to prevent the transmission of diseases or other complications. [2, 4]
How can you Prevent Chronic Kidney Disease?
Preventing CKD involves managing risk factors and maintaining overall kidney health:
Managing Underlying Conditions
- Diabetes: For individuals with diabetes, keeping blood sugar levels in check is crucial.
- Hypertension: Regular monitoring and controlling blood pressure can prevent kidney damage.
Lifestyle Modifications
- Dietary changes: Incorporating a kidney-friendly diet helps manage overall kidney function and health. This may include limiting protein intake, avoiding foods that increase blood cholesterol, and minimizing sodium and potassium intake.
- Exercise: Since obesity is a risk factor for CKD, engaging in regular physical activity is beneficial for managing the disease as it helps improve overall health and maintain a healthy weight.
- Quit Smoking: Quitting smoking improves kidney and cardiovascular health.
- Limit Alcohol Intake: Keeping the alcohol intake under 14 units a week can prevent obesity and type 2 diabetes and can ultimately prevent any damage to the kidneys over time.
- Regular check-ups: Routine medical check-up can detect early signs of CKD and other health conditions. [2, 5]
Three Common Myths About Chronic Kidney Disease
Myth 1: If You Don’t Have Symptoms, Your Kidneys Are Fine.
Fact: People often refer to CKD as a “silent disease” because it can advance without showing any noticeable symptoms. Many people don’t realize they have CKD until it is at an advanced stage. Regular check-ups and blood and urine tests are essential for early detection.
Myth 2: If you are at risk for kidney disease, there’s nothing you can do about it.
Fact: Being at risk for kidney disease does not necessarily guarantee that one will develop it. Individuals can take measures to protect their kidneys. Eating a balanced diet, engaging in regular exercise, managing blood pressure and blood sugar levels, maintaining a healthy weight, quitting smoking, and avoiding excessive use of pain medications like ibuprofen can all contribute to kidney health and reduce the likelihood of developing kidney disease.
Myth 3: Dialysis or a transplant are the only treatment options for kidney disease.
Fact: Not everyone with kidney disease requires dialysis. Because kidney disease progresses over time, it is possible to manage it in the early stages with exercise, diet, and medication. Many individuals can slow or stop the disease’s progression and maintain a normal lifestyle using these approaches. Hence, early detection and treatment play a crucial role in preventing the advancement of kidney disease. Dialysis or a kidney transplant becomes necessary only if the disease advances to kidney failure. [7]
Conclusion
Chronic kidney disease is a serious and progressive condition that requires early detection and diligent management. By understanding the risk factors, symptoms, and available treatments, individuals can take proactive steps to protect their kidney health and improve their overall well-being. Regular medical check-ups and a healthy lifestyle are key components in managing and preventing CKD.
- Chronic Kidney Disease | Johns Hopkins Medicine
- Chronic Kidney Disease (CKD): Symptoms & Treatment (clevelandclinic.org)
- Chronic Kidney Disease - StatPearls - NCBI Bookshelf (nih.gov)
- What Is Chronic Kidney Disease? - NIDDK (nih.gov)
- Chronic kidney disease - Symptoms and causes - Mayo Clinic
- Kidney Failure Risk Factor: Gender (Sex) | National Kidney Foundation
- Six Common Myths About Kidney Disease | National Kidney Foundation









